A Los Angeles-area company is preparing for the launch next year of a novel system it's calling an O-device. Resembling a cross between a C-arm and a CT scanner, Imaging3 of Burbank, CA, hopes its Dominion system will carve out a niche as a versatile mobile imaging system that takes 3D imaging to a new level.
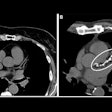
Dominion consists of an O-shaped gantry -- more like a ring than a traditional CT gantry -- mounted on a wheeled cart about the size of a mobile C-arm. Inside the gantry are an x-ray tube and a flat-panel digital detector array that rotate around the patient similar to a rotating CT tube and detector, at speeds of either 800 msec or 200 msec.
What's different is that Dominion operates using a cone-shaped x-ray beam rather than in fan-beam slices like a CT system. Proprietary software algorithms applied to the image data enable the system to create a real-time 3D image that's radiotranslucent and can be processed with standard 3D techniques.
Being able to produce 3D images in real-time rather than requiring 2D slices to be reconstructed after the exam has a number of advantages, according to Dean Janes, chairman and CEO of the company. Janes likens the system to a fluoroscopy unit that produces images in 3D rather than in 2D planes.
"You can see multiple planes simultaneously, and those are being updated simultaneously," he said. "Standard fluoro is 30 fps, which works out to 200 msec per frame or less. That is what we are giving (physicians), but we're doing it in real-time in three dimensions, so they don't have to reposition the patient. They can now see the side, back, and front view simultaneously."
Imaging3 hopes that Dominion's real-time 3D capabilities will give it great clinical flexibility that will make the system suitable for use in a variety of applications throughout the hospital. Providing image guidance for surgical intervention, in particular in orthopedics, is one such use, Janes said.
"Orthopedics will be very large since you can visualize joints in three dimensions," he said. "If it's in real-time, you can see movement in three dimensions."
Other applications could include vascular and cardiac imaging, digital radiography, and even mammography. Imaging3 will also offer a CT option that will enable Dominion to operate in what Janes calls a "CT-emulation" mode, acquiring 2D planar slices, at a fraction of the price of a new CT scanner.
Imaging3 also plans to make Dominion's mobility a selling point. Both the O-device and the system's workstation cart are mounted on wheels and can fit through a standard hospital door. The system runs off standard 120-volt power.
Janes founded Imaging3 in 1993 as an equipment refurbishing company, and the firm has expanded to offer equipment service as well as distribution of accessories such as C-arm tables. This business brings in the cash flow that's used to fund development of Dominion; Imaging3 posted revenues of approximately $2 million in 2005, Janes said. The company in January listed its stock on the Over-the-Counter Bulletin Board, under the symbol IMGG.
Imaging3 plans to install Dominion at beta sites this summer, and has a number of luminary sites lined up throughout the U.S. When the system is commercially available, Imaging3 hopes to offer the base model with real-time 3D capability at $180,000, with a device capable of CT emulation running $400,000. Dominion still requires Food and Drug Administration 510(k) clearance, and the company hopes to ship the first commercial systems in 2007.
Janes hopes the low price of the base model will be an incentive for hospitals to buy multiple Dominion units to install at various locations in the enterprise.
"Hospitals are trying to get the most value per dollar for imaging equipment, and having flexibility and having a system that can do multimodality cases is really important for them," Janes said. "We think it will help us sell more than just one per facility. Really, a hospital will at least want two or three -- one for the OR exclusively, one for trauma, and one for interventional."
By Brian Casey
AuntMinnie.com staff writer
February 6, 2005
Related Reading
Imaging3 shares begin trading, January 6, 2006
Copyright © 2006 AuntMinnie.com