Clinicians and information technology experts have made steady progress toward developing fully electronic health information systems, particularly in radiology. However, as third-generation electronic health record (EHR) systems emerged on the market in 2004, a standard clinical terminology or reference set of clinical concepts was needed to support clinical documentation, decision support, and workflow.
Standardized terminology is not used uniformly in medicine. Clinicians often use different terms to communicate the same thing or the same term to mean different things. Standardization, using a concept-based clinical terminology, resolves this situation by creating a common platform for radiologists and other practitioners to render care while allowing a basis for comparison and communication.
Standardized clinical terminology offers radiologists clarity and precision in conveying what they mean. For example, an upper GI series can be performed by either having the patient drink contrast medium or using a nasogastric tube to administer the contrast medium. Using a comprehensive standard terminology to describe these procedures allows radiologists to explicitly and accurately express the care needed for both oral and intubated studies.
Employing standardized terminology also helps define and identify patients at risk, such as those who might be allergic to contrast media, and allows for the retrieval and aggregation of more complete and useful data for analysis of patients, disease states, treatments, and outcomes -- something conventional paper records make difficult, at best.
Consider this scenario: Research indicates that women with a genetic predisposition for breast cancer benefit from additional screening with ultrasound, regardless of their breast density. Using an information system that incorporates standardized clinical terminology, a radiologist or other clinician could more readily review the medical records of patients who have a genetic predisposition for breast cancer, and recommend additional ultrasound screening.
As this example illustrates, the electronic format helps to improve quality of care by giving radiologists the ability to search for and act on risk factors that could lead to a more timely and accurate diagnosis.
Coordination and continuity of care typically necessitate that relevant information about a patient be integrated from several different clinicians and care settings. The divergent health information technology employed within and across settings, however, presents an added hurdle that must be bridged before accurate and reliable electronic communication of medical information can occur.
Standardized clinical terminology, such as Systematized Nomenclature of Medicine Clinical Terms (SNOMED CT), makes spanning this gap possible by enabling system interoperability -- that is, the capability for data to be exchanged between systems, regardless of the data architecture on which it was created. Without standardization, custom interfaces and other work-arounds become necessary, which make sharing, comparing, and retrieving patient- or population-based data within and among different information systems difficult at best, error-prone at the worst.
The importance of EHRs in radiology
Digitized data in an EHR system is fast becoming a fundamental component of modern medicine. For radiologists and other practitioners, the system offers access to critical patient-specific information. Patient-record data, such as drug allergies, co-morbid conditions, and pertinent historical information, are accessible where and when needed for complete and consistent documentation.
An EHR system facilitates effective communication within and across healthcare settings and organizations. For example, identifying patients at risk for heightened anxiety during procedures that involve a close environment, such as an MRI or CT scan, remains extremely difficult when medical records are in a paper format.
Part of the problem stems from inconsistent and incomplete documentation of the relevant patient information. An EHR system enables data to be entered in a consistent and more complete manner, which, in turn, enables it to be retrieved in a common format and used multiple times. For example, systems are typically designed with built-in prompts to remind users to enter required information. Moreover, these systems generally will not allow users to proceed unless the required information is provided.
An EHR system also allows for more efficient and efficacious care delivery among a team of primary care providers, specialists, nurses, pharmacists, and other professionals involved in patient care. Having a digitized record at your fingertips helps avoid duplicate tests and procedures, saving time and healthcare expense. Other advantages include:
- More rapid information retrieval -- depending, of course, on timely, complete, and accurate data entry
- Enhanced readability
- Reduced record-keeping costs
- Reduced or eliminated duplicate records
- Reduced storage costs
- Continuity of record keeping
An EHR system also helps create and support much-needed research databases within a healthcare enterprise. Researchers in radiology can draw upon de-identified patient data from such a database for a wide range of healthcare quality- and safety-related efforts, including:
- Quality management, such as preventing complications through more complete and more accurate preprocedural patient histories
- Outcomes studies, such as analyzing cases of delayed recovery from sedation used during a procedure
- Quality improvement projects, such as blinded double reads of imaging studies to assess consistency of interpretation
- Benchmarking and the identification of best practices, such as the dosing and monitoring of patient responses to sedation used during a procedure
- Patient safety efforts, such as reducing complications due to the use of certain contrast agents or sedation
Radiologists acknowledge that contemporary healthcare practice has grown increasingly complex, is highly information-dependent, and requires effective communication among all caregivers who treat a patient at any point in the patient's life. However, data from 2002 shows current use of EHRs at 13% for hospitals and even less for the outpatient setting.
Electronic health information in radiology, starting with an electronic radiology health record, has the potential to provide the right information to radiologists when and where they need it, thereby reducing errors, improving the quality of radiology care, helping to identify opportunities to increase the efficiency of care, and bringing about changes in radiology practice through shared knowledge.
Standardized clinical terminology: The backbone of an EHR system
Standardized clinical terminology is the content backbone of the EHR system, reducing the variability in the way data are captured, encoded, and used for the clinical care of patients and medical research.
The Institute of Medicine Committee on Data Standards for Patient Safety noted in its report that "having clinical data represented with standardized terminology and in a machine-readable format would reduce the significant (population health management) data collection burden at the provider level, as well as associated costs, and would likely increase the accuracy of data reported."
Many clinicians involved in implementing EHRs consider SNOMED CT to have distinct advantages that make it more clinically useful than other clinical terminology code sets. Developed by SNOMED International, a division of the College of American Pathologists (CAP), in collaboration with the U.K. National Health Service (NHS), SNOMED CT's controlled healthcare terminology includes comprehensive coverage of diseases, clinical findings, therapies, procedures, and outcomes. It provides the core general terminology for an EHR system, containing more than 364,000 concepts with unique meanings and formal logic-based definitions organized into hierarchies.
SNOMED CT's more than 984,000 English language descriptions or synonyms offer flexibility in expressing clinical concepts, enabling clinicians to say things in multiple ways and still be understood. Its digital repository of coded text and images creates a searchable, virtual filing system.
With more than 1.45 million relationships between clinical concepts, the core terminology makes retrieval easier, more reliable, and more consistent than plodding through paper records. And searches can be executed by any of the defining relationships within the terminology.
Consider this example: A radiologist decides to conduct a research study on blood vessel procedures and searches the SNOMED CT-driven EHRs using the phrase "blood vessels." The search results will include specialized procedures such as epidural venographies, as well as more common procedures conducted on blood vessels, such as intravenous injection. Part of SNOMED CT's power lies in the relationships built into its core clinical concepts.
Industry recognition and use
A number of prominent standards-development organizations recognize SNOMED CT's sustainable, scientifically validated terminology and infrastructure, including the American National Standards Institute (ANSI), HL7, and DICOM.
SNOMED CT is also gaining broader recognition by those working to establish core standards and terminologies for use in a U.S. health information infrastructure. As part of its efforts toward recommending patient medical record information standards, the National Committee on Vital and Health Statistics (NCVHS) recommended SNOMED CT as the general terminology for the U.S. core set for patient medical record information (PMRI) because of its breadth of content, sound terminology model, and widely recognized value.
SNOMED CT is used in a wide variety of venues and healthcare organizations so that information can be shared. These include individual clinician offices; nationwide provider organizations; government entities, such as the U.S. Department of Defense, the Centers for Disease Control and Prevention, and the National Aeronautics and Space Administration; medical research organizations; and major pharmaceutical organizations.
Industry software leaders are integrating SNOMED CT into their healthcare applications to secure system interoperability, enhance the sharing of electronic health information, and improve patient safety. For example, medical informatics software developer Cerner of Kansas City, MO, is among the vendors working to design system solutions with SNOMED CT as the backbone.
SNOMED's work with radiology organizations
Four basic principles provide the foundation for SNOMED CT and guide development activities related to the core table structure and clinical content:
- Development efforts must encompass broad, inclusive involvement of diverse clinical groups and medical informatics experts.
- The clinical content must be quality-focused and adhere to strict editorial policies to ensure scientific and clinical validity.
- The quality improvement process must be open to public scrutiny and vendor input to ensure that the terminology is truly useful within healthcare applications.
- There must be minimal barriers to adoption and use.
SNOMED CT is continuously evolving and expanding its content to incorporate clinical terminology from an increasing number of specialties. Currently, its imaging-related content provides broad representation of the procedures, drugs (such as contrast materials), anatomical structures, and findings specific to clinical imaging.
More specifically, SNOMED CT includes 2,500 imaging- and radiology-specific terms, such as CT of pelvis and radioisotope scan of bone. It also offers radiologists access to more general concepts, such as those for patient history, as well as more than 50,000 procedure concepts, many of which would be useful in documenting information in a radiology patient record.
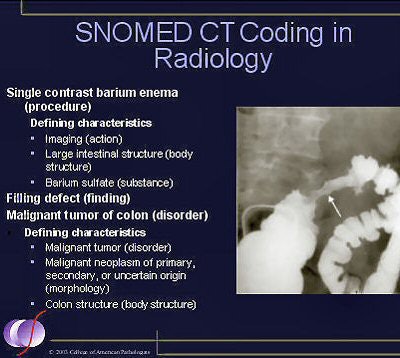
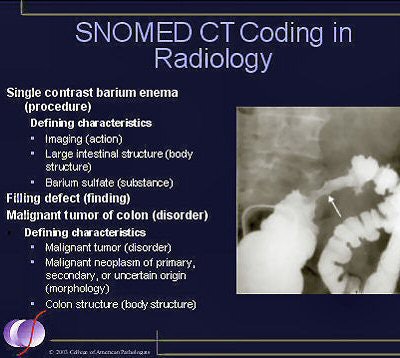 |
| SNOMED CT includes 2,500 imaging- and radiology-specific terms, as well as more than 50,000 procedure concepts that are useful in documenting information in a radiology patient record. Image courtesy of SNOMED International. |
SNOMED is continually updating its terminology to keep current with the advances of healthcare. Involvement by radiologists will help expand the overall content.
Historically, the use of various imaging modalities (MRI, nuclear medicine, ultrasound, and so on) has sometimes resulted in subtle differences in vocabularies for findings and anatomy. For example, echocardiographers might use different terminology for cardiac anatomy than nuclear medicine specialists. Through SNOMED International's collaboration with DICOM, and to an increasing degree with RSNA, it is working toward a single, convergent, widely accepted terminology representing the imaging domain.
SNOMED International also hosts the quarterly DICOM Structured Reporting Working Group meetings. As terminology content is added to the DICOM standard, it is also added to SNOMED.
The benefits of using SNOMED CT
SNOMED CT's comprehensive, scientifically validated clinical terminology makes healthcare knowledge more usable and accessible. Its core terminology enables a consistent way of capturing, sharing, and aggregating health data across specialties and sites of care. Conditions can be tagged for later retrieval.
Ultimately, it enables easy access to comprehensive information pertaining to the entire electronic health record, from medical history to chronic or acute illnesses to recent surgical procedures and treatments.
Multiple practitioners, no matter how diverse, can share important patient information, trigger effective treatment guidelines, and improve patient outcomes with the assurance that descriptions of diagnoses and treatments are represented consistently across all health care providers.
And, because SNOMED CT enables primary- and specialty-care providers and patients to share comparable data at any time, from any place, it can help to greatly reduce medical errors associated with traditional paper records.
To trigger decision support rules, different types of concepts must be linked to one another, such as drug allergies, procedures to devices, and diseases to contraindications. Many of the common rules draw on data that may be recorded at different times and places along the continuum of care, by different clinicians, and at varying levels of specificity.
For example, clinical alerts can be created based on disease and allergy coding in relation to specific medication codes. Decision support rules built on SNOMED CT enable the development of a more sensitive and sophisticated decision support system.
Because SNOMED CT facilitates interoperability between systems, its use can simplify data integration and reduce costs. Clinical care, decision support, and research, in addition to patient safety initiatives, rely on the same information; diseases, treatments, etiologies, clinical findings, therapies, procedures, and outcomes all become digitized. To foster efficiency, users can record data just once, at the level of specificity they choose, then mine it repeatedly for decision support, statistical reporting, outcomes measurement, evidence-based medicine, and cost analysis.
SNOMED CT is highly scalable and flexible, and can be used for electronic ordering of medications and lab tests, genomic databases, telemedicine, public health reporting, clinical research, disease surveillance, and consumer health information services. Moreover, the kind of data sharing enabled by SNOMED CT only increases the accuracy of clinical documentation and communication.
The breadth and depth of the terminology, as well as its computer-readable hierarchies, enable faster, reliable, and consistent retrieval of clinical information based on flexible queries. This depth allows healthcare organizations to unlock the true power of healthcare information. Cases can be retrieved based on numerous criteria, including clinical and laboratory findings, causative agents, anatomical structure, and therapeutic procedures.
Additionally, many organizations have evaluated and selected SNOMED CT as a key component of system infrastructure. This further ensures interoperability and enhances the capability to share electronic health information and improve patient safety.
Although SNOMED CT is comprehensive on its own, it can be mapped to other medical classifications and terminologies already in use, such as ICD-9 CM. This avoids duplicate data capture while facilitating enhanced health reporting, billing, and statistical analysis. SNOMED CT provides a framework to manage language dialects, clinically relevant subsets, and extensions comprised of concepts and terms unique to particular organizations or localities.
The EHR comes of age
Widespread adoption has earned SNOMED International a global reputation as a leading provider of a sustainable, scientifically validated terminology and infrastructure. Central to SNOMED CT's power are the relationships built into its core clinical concepts, which can be represented in different languages and dialects.
The promise of the electronic future has always involved making healthcare information more usable and accessible wherever and whenever it's needed to enhance quality and reduce errors and risks. SNOMED CT core content puts the consistent and reliable sharing of healthcare information within easy reach. Healthcare providers can realize this promise by employing SNOMED CT to advance excellence in patient care and safety.
By Dr. Franklin R. Elevitch
AuntMinnie.com contributing writer
April 13, 2005
Dr. Elevitch is chair of the SNOMED International Authority and is CEO of Health Care Engineering, a real-time point-of-service performance-management system firm in Palo Alto, CA. More information about SNOMED CT can be obtained online at www.snomed.org. For additional information about the role of DICOM and the RSNA in advancing the use of EHRs, visit the organizations' Web sites at medical.nema.org and www.rsna.org, respectively.
References
Board on Health Care Services, Institute of Medicine, "Key Capabilities of an Electronic Health Record System: Letter Report," July 2003.
Brailer, David J., and Thompson, Tommy G., "The Decade of Health Information Technology: Delivering Consumer-centric and Information-rich Health Care," U.S. Department of Health and Human Services, July 2004.
Hieb, Barry, "Controlled Medical Vocabulary in the CPR Generations, ID number TU-20-1272," Gartner, November 2003.
National Committee on Vital and Health Statistics, "NCVHS Recommendations for PMRI Terminology Standards," November 2003.
Related Reading
Donnelly named SNOMED VP, September 15, 2004
U.S. makes SNOMED available through library, May 7, 2004
HHS removes obstacles to paperless health system, July 2, 2003
PointDx adds SNOMED to REX, June 4, 2003
RSNA's RadLex initiative gathers momentum, December 27, 2002
Copyright © 2005 SNOMED



















