As the 37.5 million male baby boomers march into the latter decades of their lives, inevitably the prevalence of prostate cancer will escalate. According to the Prostate Cancer Foundation, while only one in 10,000 men under the age of 40 receives a diagnosis of prostate cancer, the rate increases to one in 30 for men between the ages of 40 and 59, and soars to one in 14 as men reach the decade of their 60s.
The National Cancer Institute estimates 219,000 new prostate cancer diagnoses in 2007, with 27,000 deaths anticipated from the disease.
Treatment for this condition is complex and multifaceted, with wide-ranging options available for most patients. Most urologists favor total resection of the prostate as the only way to cure early stage lesions, but they enter into collaboration with radiation oncologists in an attempt to reduce the very negative side-effects of potential incontinence and impotence that may result from radical prostatectomy. Refinements to the various alternatives are destined to increase in effectiveness while diminishing the sequelae that treatment can yield.
The diverse treatment methodologies for prostate cancer are explored in a report published this month entitled "Trends in the Prostate Cancer Treatment Market: 2007 and Beyond," published by IMV Medical Information Division of Des Plaines, IL. The report explores prostate cancer treatment from the perspective of both urologists and radiation oncologists, with an eye to the future as the discipline evolves.
The report was compiled through 237 surveys, conducted online and through personal interviews, with 122 completed by urologists and 115 by radiation oncologists. In both instances, respondents were engaged in private practice across the U.S.
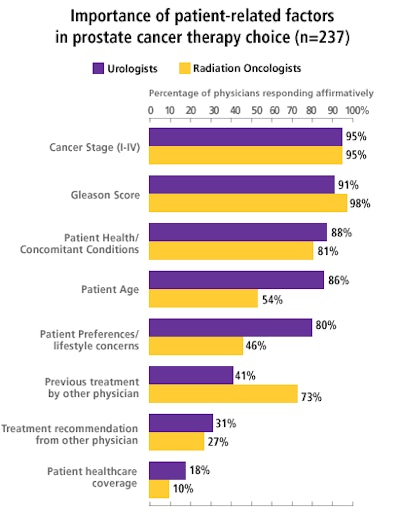
A variety of treatment options lie before the decision-making team, which typically includes the urologist, the radiation oncologist, and the patient. Treatment decisions are driven by a number of factors that include patient age at diagnosis, stage of the disease, and the Gleason score that measures relative aggressiveness of the tumor cells.
Possible treatment pathways that may be applied either singly or as a combination of several modalities include:
- Surgical removal of the prostate, through either an open surgical field or laparoscopic techniques with or without robotic assistance
- Radiation-based treatment with external-beam radiation therapy (EBRT)
- Internal radiation treatment with either permanent low-dose radiation brachytherapy seed implants or high-dose radiation pellets that are inserted and removed
- Cryotherapy that involves freezing the prostate and surrounding tissue
- Hormonal therapy, such as testosterone suppressant therapy
 |
Combination therapy
Frequently, the patient receives a combination of therapies such as neoadjuvant treatment with hormonal agents, either pretreatment or concurrent with radiation treatment, according to Mary Patton, director of online market research at IMV.
"Almost 70% of urologists and 88% of radiologists say that the most likely combination of therapies used by both urologists and radiation oncologists are EBRT plus hormonal," Patton said.
Reviewing the patient side of the equation, these radiation oncologists estimate that half of their patients with prostate cancer undergo combination therapy, while the urologists report that 39% of their patients would receive combined management of their disease. Patton explained that the percentage is lower for urologists because when they remove the prostate, combination therapy would no longer apply.
EBRT
Virtually all of the radiation oncologists in the survey sample have access to a linear accelerator with intensity-modulated radiation therapy (IMRT) capabilities. IMRT provides increased radiation dosage to the tumor while sparing surrounding tissues through use of a multileaf collimator that modifies the beam.
 |
Slightly over half of these same physicians have access to image-guided radiation therapy, which offers daily CT guidance of treatment to the target area to add precision to the technique.
"IGRT is not a replacement for IMRT, it is additive," Patton said. "The reason more people aren’t doing IGRT is due to lack of access to the technology."
Among the radiation oncologists who responded to the survey, 58.3% expect greatly increased use of IGRT in three years, and 25% expect to see similar growth in IMRT utilization over the same time period.
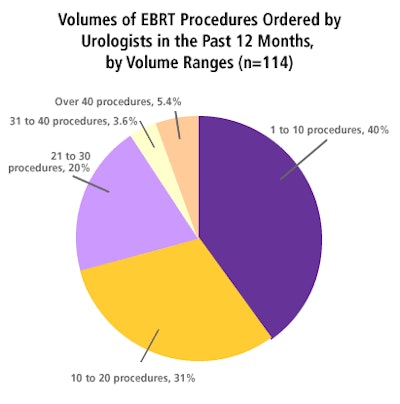
Considering that external-beam treatment must be ordered by urologists to be accomplished by radiation oncologists, this graph depicts referral patterns among the survey sample of urologists.
| Summary: Monthly total prostate cancer visit statistics (n = 237) | |||
 |
|||
| Respondent Specialty | Urologist | Radiation Oncologist | Overall |
 |
|||
| Total for all respondents | 7,630 | 3,984 | 11,614 |
 |
|||
| Mean | 62.5 | 34.6 | 49.0 |
 |
|||
| Median | 50.0 | 25.0 | 40.0 |
 |
|||
| Standard deviation | 48.7 | 27.9 | 42.3 |
 |
|||
| Maximum | 400.0 | 150.0 | 400.0 |
 |
|||
Brachytherapy
Implanting permanent low-dose brachytherapy seeds, roughly the size of a grain of rice, in the prostate has become the treatment of choice for many patients. This technique usually involves close collaboration between the urologist and radiation oncologist. The IMV survey asked respondents to rate product quality, pricing, customer service, and perceived efficacy of brachytherapy seed implants from eight different vendors.
Patton noted that even though the urologist is charged with performing the procedure itself, the choice of brand of implant seeds is left entirely up to the radiation oncologist. That said, in terms of overall awareness, she reported that the three seed vendors who scored highest were Bard Urological (ProSeed), Theragenics (TheraSeed), and Oncura (OncoSeed) among the radiation oncologists.
Another form of brachytherapy, high-dose radiation (HDR), is accomplished over a span of several days. Initially the patient under anesthesia has multiple catheters placed in the perineum, through which high-dose radioactive pellets are introduced and then removed after a brief period of time. While there are perceived advantages in the ability to provide very precise dose distribution, many clinicians feel the disadvantages in terms of equipment and difficulty in maintaining catheter placement may outweigh the positive aspects of this technique.
In the IMV survey sample, about half of the urologists and 20% of the radiation oncologists had ordered or performed HDR, but most of them had done only one to three procedures a year. Patton explained that there could be a timing issue involved in the survey results, since this technology is relatively new.
Surgical intervention
The preference among most urologists is surgical removal of the prostate, but significant side effects such as incontinence and impotence temper enthusiasm among patients.
The latest push is towards the use of nerve-sparing techniques via minimally invasive laparoscopic surgery designed to reduce those life-altering side effects that are common with the traditional approach. Robotic-assisted procedures form the very latest development in laparoscopic surgical removal of the prostate.
New directions
According to the survey, 27% of respondents either order or perform cryotherapy, a technique of tumor ablation through freezing the tissue. However, Patton noted that the disadvantages to this technique include some of the same negative side effects as surgery, meaning it probably has limited utility as a primary modality.
Proton beam radiation therapy (PBRT) shows promise, but the availability of this technology is quite limited due to the expense of the treatment systems. There are currently only six centers in the U.S. engaged in this form of EBRT, and many use it only for the most difficult prostate cancer cases in patients with the highest Gleason scores.
Eye to the future
When asked where they thought prostate cancer treatment would be in five years, one respondent predicted that more than 90% of radical prostatectomies would be performed using robotic equipment in minimally invasive laparoscopic procedures.
Radiation oncology respondents voiced serious concerns about future reimbursement issues, and predict more "watchful waiting" until the disease progresses to a higher stage before treatment occurs, according to the IMV results.
By Cheryl Hall Harris, R.N.
AuntMinnie.com contributing writer
August 9, 2007
Related Reading
Computer-assisted MR guidance improves prostate biopsy, July 31, 2007
Real-time elastography accurately detects prostate cancer, July 30, 2007
Black men underestimate prostate cancer risk, June 15, 2007
Soy isoflavones may boost efficacy of radiotherapy for prostate cancer, June 15, 2007
Prostate cancer treatments yield different quality-of-life outcomes, June 11, 2007
Disclosure notice: AuntMinnie.com is owned by IMV, Ltd.
Copyright © 2007 AuntMinnie.com



















