From perfusion imaging to infarct detection and guided intervention, cardiac MRI (CMRI) is gaining utility and fans in the academic world and beyond. The options are poised to expand rapidly in the coming years thanks to better coil designs, higher field strengths in scanners, and specialized contrast agents, to name a few of the forces shaping CMR's future.
At the Integrated Imaging in Clinical Cardiovascular Practice meeting in San Francisco last month, Dr. Christopher Kramer touched on a panoply of emerging applications for MRI. Kramer is a professor of radiology and medicine, and director of cardiac MRI at the University of Virginia Health System in Charlottesville.
Topping the list of emerging technologies are scanners with higher field strengths, in current clinical settings at 3 tesla, with investigation ongoing at much higher strengths.
With its improved signal-to-noise ratio, 3 tesla "is likely to be better for applications that at this point are signal-starved, including perfusion and coronary imaging," Kramer said.
But 3-tesla systems have further development ahead of them before they can replace 1.5-tesla systems for routine clinical use, he said.
"The downside of higher field strength is that it's not as good for bread-and-butter functional imaging -- that is, steady-state free-precession imaging, which is the ... way we image LV (left ventricular) structure and function right now," Kramer said. "At higher field strengths there are more artifacts. There are also issues with ECG gating. Hence in 2006, 1.5 tesla is really the platform of choice for cardiac imaging."
But the situation may well change in one to three years, as 3-tesla scanning is further developed, and the problems associated with its use are solved, he added.
Parallel imaging coils
Massively parallel imaging is another key technical advancement, in which a multielement coil is placed over the patient's chest and on the table. Most current scanners have eight or 16 elements per coil, but the latest 32-channel torso coil extends functionality further.
"What do additional channels do? Basically, they allow you to use advanced computer processing to obtain signal from multiple areas of the chest, and at the same time integrate that signal," which in turn enables significantly faster acquisition times and improved signal-to-noise ratios, Kramer said. Most scanners purchased today have the ability to do parallel imaging with multiple coils.
 |
| 32-channel radiofrequency torso coils for massively parallel cardiac MRI. All images courtesy of Dr. Christopher Kramer. |
Tagging for functional imaging
Another MRI advance, real-time imaging, has improved the assessment of LV function, Kramer said. This feature has actually been available for a while, but the limitation has been that most acquisitions are still ECG-gated, and many patients can't hold their breath. Real-time imaging doesn't depend on breath-holding, and the technique is not impeded by arrhythmias. But the price is lower resolution, he said.
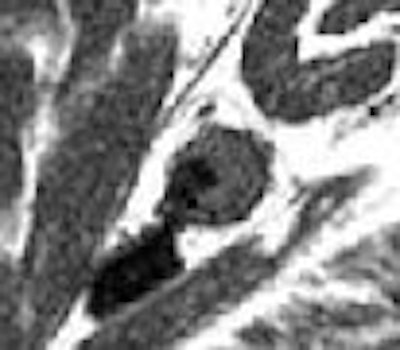
Myocardial tissue tagging is one way of improving spatial and temporal resolution, but new techniques are in development. Research on one method, cine displacement encoded stimulated echo, or cine DENSE, is being led by Kramer's colleague, Frederick Epstein, Ph.D., at the University of Virginia (Radiology, March 2004, Vol. 230:3, pp. 862-871; Magnetic Resonance in Medicine, October 2004, Vol. 52:4, pp. 774-81).
Cine DENSE imaging "is so much simpler than speckle tracking in echo; it has very high spatial and temporal resolution," Kramer said. An example of the technique showed the displacement of individual pixels in the short axis of the LV in a normal volunteer in both two and three dimensions. From this data a strain map can be created to assess, for example, circumferential strain during the cardiac cycle.
"This kind of imaging can be done here and now" -- for example, in a patient with LV dyssynchrony in congestive heart failure, Kramer said. "It's very useful for demonstrating regional function. What's coming in the next two to three years is the ability to see strain maps in real-time while you're imaging the patient."
In a patient-imaged postmyocardial infarction, overlaid color-coded maps showed the infarcted region, accompanied by displacement and strain maps. The dysfunction extended "well beyond the clearly delineated infarct border into the lateral margins and subendocardial borders," Kramer said, "showing why we can't image regional function the size of the myocardial infarction because the dysfunction extends clearly beyond the infarct border."
 |
| 2D cine DENSE imaging is a breath-hold cine magnetic resonance pulse sequence based on displacement encoding with stimulated echoes (DENSE) for quantitative myocardial motion tracking. An early study in 12 healthy volunteers yielded spatial resolution and temporal resolution of 2.7 x 2.7 mm and 60 msec, respectively, and the results were well correlated to conventional MR tagging (Radiology, March 2004, Vol. 230:3, pp. 862-871). Use of spatial modulation of magnetization for time-independent artifact suppression minimized artifact-generating echo during systolic imaging to 10% or less of the total cine DENSE energy, further in subsequent studies, with results displayed in 3D. |
Stress and perfusion advances
Stress imaging can also be performed with standard steady-state free-precession imaging, yielding excellent image quality with 10-20 msec temporal resolution, even at heart rates as fast as 150 bpm. MR tagging can also assess regional function at stress, Kramer said.
As for perfusion imaging, some development work is being performed on 3-tesla scanners, he said, but to some extent the development of parallel coils has obviated the need for higher field strengths.
"Parallel imaging has sped up the acquisition, and that's what has limited to date perfusion imaging," Kramer said. "I think that right now we're very comparable to nuclear -- and making some strides above and beyond it -- in terms of coverage and spatial resolution."
Late gadolinium enhancement, already robust, is being advanced with the use of phase-sensitive inversion-recovery imaging. Traditionally, this technique has required the technologist to choose an inversion time in order to "null" normal myocardium, Kramer said. But with phase-sensitive inversion recovery, the inversion time is chosen automatically, he said. Late gadolinium enhancement combined with parallel processing opens up new opportunities in 3D imaging that can provide invaluable prognostic information.
A recent study examines the prognostic implications in late gadolinium enhancement in patients with dilated cardiomyopathy, Kramer said. The group found that "even the smallest area of late gadolinium enhancement -- the smallest prior infarct even if unknown -- was very important prognostically," he said. "The presence of any infarct -- no matter how small -- predicted event-free survival and overall survival" (Circulation, July 2006, Vol. 114:1, pp. 32-39).
Some have argued against the use of late gadolinium enhancement, Kramer added, but this study proves its value in even the smallest infarct, and more broadly as a manifestation of coronary artery disease activity, he said.
Advances in signal-to-noise ratios have sharpened the images, he said, and other techniques are aimed at making MRI "more CT-like," at least in terms of resolution, Kramer said.
"We really don't have the spatial resolution of CT, and that's really a disadvantage of MR," he said. "CT clearly has advantages in terms of coronary imaging at present."
Weber et al engaged the issue of resolution with whole-heart steady-state free-precession coronary artery magnetic resonance angiography (MRA). Three thin-slab volumes are acquired with the method, and so-called navigator echoes are used to track heart motion, Kramer said.
The authors found that the technique improved visible vessel length, and facilitated high-quality coronary MRA of the complete coronary artery tree in a single measurement (Magnetic Resonance in Medicine, December 2003, Vol. 50:6, pp. 1,223-1,228).
Plaque imaging advances
Kramer, Isbell, and colleagues are working on high-resolution imaging of plaque volume in the superficial femoral and carotid arteries as a marker of developing atherosclerotic disease.
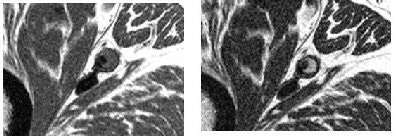
In the carotid arteries of one patient, T1-weighted imaging showed plaque burden homogeneously, while T2-weighted images showed different plaque components: fibrous cap, dark lipid core in the adventitia, and a dark crescent indicating a calcium deposit, Kramer said.
"With the patient lying quietly on the table, (MRI) may be quite competitive with sticking a catheter in a coronary artery and doing vascular ultrasound to measure plaque volume," he said.
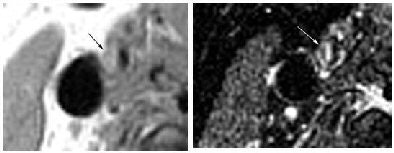 |
| Images of carotid artery above show (left) a T1-weighted inversion-recovery black blood spin-echo image showing plaque burden. At right, a T2-weighted image (also inversion-recovery black blood spin-echo) shows plaque components, including the bright fibrous cap along the luminal surface and the darker lipid core toward the adventitia. |
 |
| Images of a superficial femoral artery were acquired with an inversion-recovery black blood spin-echo sequence. The T1-weighted image (left) demonstrates plaque burden, and the T2-weighted image (right) shows the bright luminal tissue, which likely represents thrombus and/or fibrous tissue, and the darker tissue, which is the lipid core. |
"We can image the coronary wall, but for morphology, not plaque components," Kramer said. "We just don't have the spatial resolution yet." But there may be a solution in new contrast agents. Gadolinium-based fibrin-binding contrast agents, for example, brighten areas of thrombosis that cannot be detected otherwise.
Interventional MR is an attractive concept thanks to MRI's excellent soft-tissue contrast. Researchers at the University of California, San Francisco (UCSF), and elsewhere are taking steps toward real-time interventional MRI. At UCSF, a sliding table ferries patients from the angiography table, where catheters are inserted, to an adjoining room where MRI performs the imaging. This is just an interim step; as soon as the new MRI-compatible catheters can be deployed, the sliding table will be unnecessary, Kramer said.
MR-compatible hardware expands therapeutic options
Raval et al from the National Institutes of Health (NIH) performed real-time MRI-guided stent placement in an aortic coarctation model with 13 pigs, using commercially available catheters.
"Follow-up catheterization and necropsy showed accurate stent deployment, durable gradient reduction, and appropriate neointimal formation," the group wrote. "MRI immediately identified aortic rupture when oversized devices were tested" (Circulation, August 2005, Vol. 112:5, pp. 699-706).
As for MR safety, existing pacemakers and defibrillators are being tested for MR compatibility and postimaging function, while new MR-compatible devices are being developed from scratch.
"There is some artifact, but ultimately many devices are safe," Kramer said. "Defibrillators are being studied in animal models and some may be safe. More research is needed." A new MR-compatible pacemaker will be deployed this fall.
"I think it's a very exciting time in the field," Kramer said.
By Eric Barnes
AuntMinnie.com staff writer
September 11, 2006
Related Reading
MDCT complements MR in heart disease evaluation, August 22, 2006
MDCT, SPECT, and echo agree on LV function August 7, 2006
MRI characterizes myocardial tissue in all its states, June 2, 2006
Cardiac imaging dazzles, but radiologists can't compete alone, April 10, 2006
MDCT maybe equivalent to MRI, tops echo and SPECT for heart function, February 15, 2005
Copyright © 2006 AuntMinnie.com