MRI is considerably more sensitive than mammography for detecting multiple malignant foci in women with extremely dense breasts, according to a study in the American Journal of Roentgenology. However, the modality doesn’t quite hit the mark in women with fatty breasts.
Catching multifocal, multicentric disease is especially important because relapse, even after mastectomy, occurs quite often, explained Dr. Francesco Sardanelli and colleagues. Based on pathology-controlled studies, multifocal (one quadrant involved) or multicentric (two or more quadrants) cancer occurs with a frequency of 14% to 47% of cases. But the sensitivity of mammography for detecting multiple malignant foci is often less than 50%.
"The aim of our study was to compare mammography and MRI ... for multiple breast cancer foci in potential candidates for mastectomy using the whole-breast pathologic examination as a gold standard," the group wrote (AJR, October 2004, Vol. 183:4, pp. 1149-1157).
Sardanelli is from the Istituto Policlinico San Donato in Milan, Italy. He and his co-authors are participating in the Italian Trial for Breast MR in Multifocal/Multicentric Cancer, sponsored by the Italian Association for Medical Radiology and Bracco Imaging of Milan.
The study population consisted of 90 women who had proven breast cancer and a planned mastectomy. Dynamic MR was performed and precontrast images were obtained using a 3D spoiled gradient-echo coronal sequence. Postcontrast imaging was done after an intravenous injection of gadoteridol (ProHance, Bracco Imaging) at a dose of 0.1 mmol/kg at 2 mL/sec. The MRI protocol included a slice thickness of 3 mm or less with no interslice gap covered by both breasts.
 |
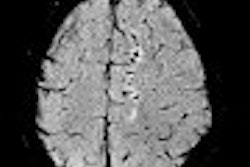
| Forty-seven-year-old woman with multicentric breast cancer in dense breast. Mediolateral oblique mammogram does not show clear depiction of tumor. Sardanelli F, Giuseppetti GM, Panizza P, Bazzocchi M, Fausto A, Simonetti G, Lattanzio V, Del Maschio A, "Sensitivity of MRI Versus Mammography for Detecting Foci of Multifocal, Multicentric Breast Cancer in Fatty and Dense Breasts Using the Whole-Breast Pathologic Examination as a Gold Standard," (AJR 2004; 183: 1149-1157). |
Breast lesions were located using a nine-region map, comprised of eight regions and the nipple region. Using this map, comparison of the location of the breast foci at pathology, mammography, and MRI was done by two radiologists in consensus. A third radiologist matched the findings from mammography and MR with the pathologic reports.
Based on the pathology results in 99 breasts, there were 188 malignant foci in total (52 unifocal cancers, 29 multifocal, and 18 multicentric) with 158 invasive cancers and 30 in situ.
The global sensitivity of MRI for cancer detection was 81% versus 66% for mammography. For the detection of invasive foci, MRI's sensitivity was 89% and mammography's was 72%. The sensitivity for the two modalities was close for in situ foci -- 40% versus 37%.
 |
| Same patient. Contrast-enhanced subtracted coronal MR image (first dynamic phase) shows not only major tumor as large round area of contrast uptake with irregular borders at external quadrants, but also three small satellite foci (arrows) showing multifocal cancer. Sardanelli F, Giuseppetti GM, Panizza P, Bazzocchi M, Fausto A, Simonetti G, Lattanzio V, Del Maschio A, "Sensitivity of MRI Versus Mammography for Detecting Foci of Multifocal, Multicentric Breast Cancer in Fatty and Dense Breasts Using the Whole-Breast Pathologic Examination as a Gold Standard," (AJR 2004; 183: 1149-1157). |
"Mammography missed a total of 64 malignant foci compared with a total of 36 malignant foci missed on MRI," the authors wrote. The misses on MR may have been the result of inadequate spatial resolution, the group said, basing their hypothesis on the diminutive size of these foci, a median diameter of 5 mm versus 8 mm for detected foci.
The global positive predictive value (PPV) was 68% for MRI and 76% for mammography. The latter may have turned in a higher PPV because of selection bias. Both expert observers were aware of the entry criteria (planned mastectomy) for this study.
"In other words, they looked for as many as possible findings attributable to malignant foci on the mammograms," explained Sardanelli in an email to AuntMinnie.com. "An associated result was the mammogrphic detection of all the nine cases of bilateral breast cancer."
The same may not hold true in a clinical setting, when radiologists are not necessarily aware that radical surgical treatment is planned, he added.
"This high performance of mammography can be regarded as a theoretical high limit for searching multiple malignat foci with this technique," he said.
In breasts with a fatty pattern, MRI's sensitivity was 80% for detection compared with 75% for mammography, which was not statistically significant. The PPVs for MRI and mammography in fatty breasts -- 65% and 73%, respectively -- also did not reach statistical significance.
"Despite the fact that MRI is the best technique available for the detection of multifocal, multicentric breast cancers, improved performance may still be achievable," the authors wrote. Using higher in-plane and through-plane spatial resolution could improve MRI's sensitivity. Specificity could be boosted with proton MR spectroscopy to integrate morphologic and dynamic data.
The group concluded that in nonfatty breasts, dynamic MRI results could reduce the number of inadequate surgeries in which malignant foci are not completely removed, paving the way for relapse.
Participants in the Italian trial are currently discussing research on MR as a preoperative study for breast cancer patients, Sardanelli said.
"We know from previous experience that MR changes therapy planning in about 15% of the cases, enlarging the number of mastectomies in a nonnegligible fraction of cases. However, the local relapse rate at five years is not over 7%-8% (and lower in recent trials)," he wrote. "The challenge is to use MR avoiding an overtreatment...MR could be used for a woman-by-woman tailored treatment."
However, instituting an MR-based, presurgical protocol would require a team approach between radiologists, surgeons, and oncologists, Sardanelli added.
"We need a consenus...on this matter. Only after, we can examine the possibility of a new study aimed at evaluating the advantages of performing a preoperative MR for breast cancer in terms of reduced number of local recurrences and better survival rate," he explained.
By Shalmali Pal
AuntMinnie.com staff writer
October 13, 2004
Related Reading
MRI best for women with heredity risk of breast cancer, September 15, 2004
MRI breast cancer test benefits high-risk women, July 29, 2004
NSECT may trump traditional imaging by spotting breast cancer before it manifests, July 28, 2004
MRI shows strength in breast tumor detection and quantification, June 7, 2004
Copyright © 2004 AuntMinnie.com