Two years ago, U.K. clinicians set out to find an optimal method for imaging lymphatic vessels of the upper limb. They determined that intradermal injection provided rapid deployment of radiotracers to lymphatic vessels, making it ideal for imaging lymphatic morphology.
They also found that Tc-99m human immunoglobulin (Tc-99m-HIG) was generally superior to nanocolloid for this purpose (European Journal of Nuclear Medicine and Molecular Imaging, April 2004, Vol. 31:4, pp. 555-563).
But does this intradermal injection method work as well in a more challenging situation, such as the severely swollen upper limb of breast cancer-related lymphedema? Those same researchers sought the answer to that question with a new study in the American Journal of Roentgenology.
"It is not universally accepted that intradermal injection is the preferred technique for routine lymphoscintigraphy. This is partly because the principal clinical indication for lymphoscintigraphy is investigation of a swollen limb of unknown cause," wrote Dr. Susan O'Mahony and colleagues. "The purpose of the current study was ... to see whether the superiority of the intradermal route was maintained in the setting of severe edema of the subcutis" (AJR, May 2006, Vol. 186:5, pp. 1349-1355).
O'Mahony and several of her co-authors are from the department of nuclear medicine and the Cambridge Breast Unit at Addenbrooke's Hospital in Cambridge, U.K. Other contributors are from St. George's Hospital in London and the Royal Sussex County Hospital in Brighton, U.K.
Their patient population consisted of six women with breast cancer-related lymphedema who had undergone surgery about five years earlier. Duration since the onset of swelling was a mean of four years. The Tc-99m-HIG was injected subcutaneously and interdermally using a 30-gauge needle. Both injection techniques were performed with the patient's metacarpophalangeal joints flexed.
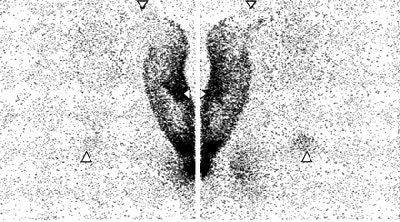 |
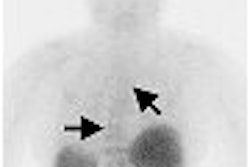
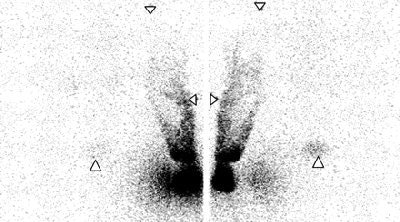
| Lymphoscintigraphy images of upper limb and torso in female patient. Downward-pointing arrowheads = shoulders, lateral arrowheads = elbows, upward-pointing arrowheads = pubic bone. Images obtained 52 and 48 minutes after intradermal (above) and subcutaneous (below) injections, respectively. There is greater clarity and earlier visualization of lymphatic structures after intradermal injection. Left and right panels are posterior and anterior images, respectively. |
 |
| O'Mahony S, Solanki CK, Barber RW, Mortimer PS, Purushotham AD, and Peters, AM, "Imaging of Lymphatic Vessels in Breast Cancer-Related Lymphedema: Intradermal Versus Subcutaneous Injection of 99mTc-Immunoglobulin" (AJR 2006; 186:1349-1355). |
Imaging was done with a double-headed, rectangular field-of-view gamma camera (Helix SPX, Elscint, Haifa, Israel). Patients were imaged on two occasions, one to six weeks apart. Images were evaluated by a nuclear medicine physician. The scintigraphic features evaluated were clarity and speed of visualization of lymphatics, speed of the radiotracer's transit to the axilla, and speed of appearance and prominence of blood pool signal.
"Lymphatic structures were visualized earlier and with unequivocally greater clarity after intradermal injection compared with subcutaneous injection in all six patients," the authors wrote. In addition, discrete lymphatic vessels in the upper arm were seen in five patients after intradermal injection.
No clear difference was seen between the two techniques with respect to activity outside the depot, they stated. However, arm activity steadily increased after subcutaneous injection, while after intradermal detection, arm activity reached a peak and then declined.
Finally, the recovery injected Tc-99m-HIG in venous blood was greater after the intradermal method in all six patients. "The more rapid delivery of radiotracer to the lymphatic system that underlies the superior imaging obtained from intradermal injection is reflected in a higher blood recovery," the group concluded.
Breast cancer-related lymphedema affects 20% to 25% of women who undergo axillary lymph node clearance. Treatment of the axilla with surgery and/or radiation therapy can lead to edema. The authors explained that the findings have implications for imaging lymphatic vessel regeneration and rerouting.
By Shalmali Pal
AuntMinnie.com staff writer
May 10, 2006
Related Reading
Predictive index improves criteria for postmastectomy radiation selection, April 26, 2006
Automated assay detects metastatic breast cancer in sentinel lymph nodes, March 22, 2006
Ultrasound shows potential for sentinel lymph node detection, May 12, 2005
Copyright © 2006 AuntMinnie.com