With a relapse rate as high as 40%, colorectal cancer patients clearly need better preoperative assessment. Australian researchers investigated whether FDG-PET could be the modality to pick up where conventional imaging, and CT in particular, leaves off. Their results were published in the Journal of Nuclear Medicine.
"The utility of PET in routine clinical practice will likely depend on its ability to provide incremental information compared with CT in selected patients rather than serve as a replacement for CT...The current study prospectively examines the clinical impact of F18-FDG-PET on the management of recurrent colorectal cancer," wrote Dr. Rodney Hicks from the Peter MacCallum Cancer Institute in East Melbourne. Hicks’ co-authors were Victor Kalff, Robert Ware, David Binns, Allan McKenzie, and Annette Hogg, Ph.D. (JNM, April 2002, Vol.43:4, pp. 492-499).
The study included 102 patients, all of whom were potential candidates for aggressive therapy if localized disease was confirmed. The original tumor location was in the rectum in 36% of the cases, the rectosigmoid colon in 22%, the cecum in 12%, the transverse colon in 9%, the ascending colon in 9%, the sigmoid colon in 6%, the descending colon in 4%, and unspecified in 2%.
On the routine clinical request form, the referring physician was required to state the following:
- Indication for the PET scan.
- Histology of the tumor.
- Clinical stage.
- Results of most recent structural imaging tests.
- Proposed management plan up to the time of referral.
All but six of the physicians stated their prospective management plans.
A CT scan was performed within two months of PET in 89% of the cases. PET scanning was performed on a Quest 300H (GE Medical Systems, Waukesha, WI). To reduce out-of-field scatter in the 3-D mode, patients were catheterized when possible and given 10-20 mg of furosemide 30 minutes beforehand. Imaging was done at least one hour after intravenous injection of 70-120 MBq of 18F-FDG.
"The PET stage was determined by incorporating the PET findings with all other staging information, and was abstracted from the clinical report issues thereafter. All referring physicians were contacted within one month of the scan," the group wrote.
The PET study was deemed true positive if recurrent disease was confirmed at surgery or on subsequent follow-up. A false positive was defined as either misclassification of benign abnormality or abnormalities that showed no progression after two years of follow-up. PET results were considered true negative if the patient had no disease progression at least a year later. A false negative meant that no malignancy had been seen on PET, but was found by surgery or conventional imaging.
According to the results, FDG-PET information directly changed the management of 56% of 96 patients. For the six patients whose referring oncologist declined to state a preoperative management course, PET results yielded two true negatives and four true positives.
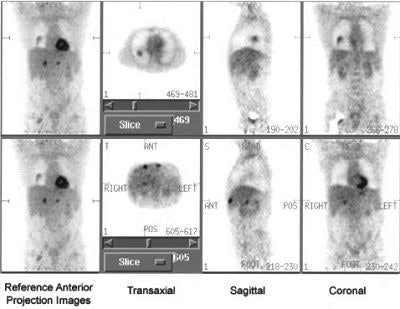
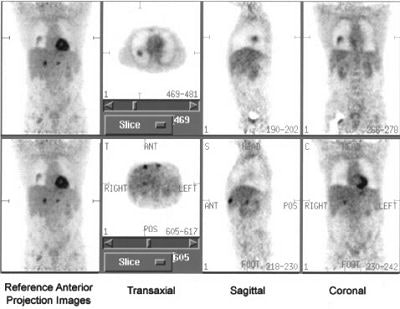
 |
| Both CT and FDG-PET suggest the presence of single hepatic metastasis. At laparotomy, additional small (<1 cm) metastases were found, and hepatic resection was abandoned. |
In total, PET changed 59% of the management decisions in a total of 102 patients. The most frequent change was to vary the active treatment planned, the authors wrote. Surgical intervention plans were jettisoned in 43 patients (60%) because of PET results. PET also influenced a change from observation to active therapy in 12 patients.
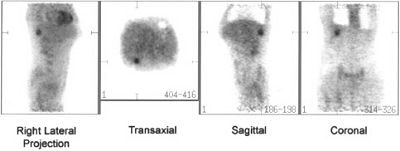
 |
| This patient was being considered for resection of an apparently isolated lung metastasis. In addition to the lung lesion (top), FDG-PET found additional multiple liver metastases that were not apparent on CT (bottom). Surgery was avoided, and abdominal metastases were subsequently confirmed by serial imaging. Images courtesy of the Journal of Nuclear Medicine. |
"The high impact of PET was particularly evident in the group of patients with apparently limited metastases for whom surgical resection was planned. In this group, only 10 came to operation, including two for whom the PET findings of inoperability were confirmed," they wrote.
But PET did have some limitations. First, most false-negative results were related to lesions of < 1 cm that were eventually documented through invasive procedures many months after the scan. In addition, the final management of some patients was inconsistent with the imaging findings. In two patients, PET identified disease relapse but underestimated the extent of disease. In nine patients, the PET results were correct for the presence and extent of relapse, but these results were "inappropriately ignored" by referring clinicians, Hicks said.
"At the time that this study was commenced, some clinicians had relatively little experience with the role of FDG-PET in colorectal cancer, and some felt uncomfortable denying patients potentially curative treatment on the basis of PET results that were discordant with conventional imaging," Hicks wrote in an e-mail to AuntMinnie.com.
Of these nine cases, eight had extrahepatic disease on FDG-PET that was confirmed by laparotomy prior to planned hepatic resection. In one case, PET results were recognized prospectively to be false negative with a new <1-cm hepatic metastasis on CT that was not seen on PET. In that instance, surgery proceeded due to the absence of evidence of extrahepatic disease, Hicks added.
Overall, surgery was canceled in 60% of the cases because of PET findings. The group concluded that PET documents widespread disease and can be used to reliably redirect patients to nonsurgical therapy.
A hybrid PET-CT scanner has recently been installed at the Peter MacCallum Cancer Institute. Hicks and his group are now evaluating the independent and incremental role of PET in recurrent colorectal cancer.
"Our initial experience suggests that PET-CT particularly aids in the differentiation of physiological bowel wall uptake from peritoneal disease," he said.
By Shalmali PalAuntMinnie.com staff writer
May 7, 2002
Related Reading
For doctors in the know, FDG-PET alters colorectal cancer management, April 10, 2001
PET imaging is cost-effective in management of recurrent colorectal cancer, April 2, 2001
Copyright © 2002 AuntMinnie.com




















