SAN FRANCISCO - A growing body of evidence is showing that plaque morphology is even more important than degree of stenosis in predicting outcomes of percutaneous coronary intervention (PCI). But precisely which imaging methods are the most effective, and ways in which they can improve interventional outcomes, still needs clarification.
To begin, the PROSPECT (Providing Regional Observations to Study Predictors of Events in the Coronary Tree) study, presented on Thursday at the 2009 Transcatheter Cardiovascular Therapeutics (TCT) meeting in San Francisco, represents a major boost to advocates of pretherapeutic plaque morphology imaging.
Dr. Gregg Stone from Columbia University Medical Center In New York City and colleagues at 40 centers worldwide followed nearly 700 patients for three years after plaque assessment with ultrasound-based VH - IVUS imaging (Volcano, San Diego).
Over a three-year follow-up period, vulnerable lesions, identified as VH IVUS having more than 10% thin-cap fibroatheroma area (TCFA) were far more likely to produce adverse events than stable lesions (hazard radio of 3.8 [p<0.0001] versus 0.2 for [pathological intimal thickening (PIT)] lesions).
A day before the new study was announced, Dr. Sergio Waxman discussed how initial plaque morphology helps doctors better plan PCIs, how various interventions have been found to affect vessel morphology, and how they can potentially reduce the number of interventions that fail due to poor choices in PCI technique. Nearly any pre-PCI assessment would be an improvement on the current standard of care, Waxman said.
"Plaque morphology prior to PCI is very diverse; however, the treatment paradigm is the same regardless of different plaque morphology or the extent of disease," said Waxman, from the Lahey Clinic in Burlington, MA, and Tufts University School of Medicine in Boston.
Vessels containing various plaque morphologies -- from stable lesions to thin-capped fibroatheromas, ruptured plaques, and focal and diffuse disease -- all respond very differently to different stenting, he said.
"The healing response depends partly on the substrate of the plaque, and stented lesions in unstable plaques are prone to rupture," Waxman said, citing Finn et al, who found very different healing patterns in different plaque morphologies after PCI.
"In addition to its role in facilitating incomplete apposition, plaque morphology may also affect the rate of healing of the stented segment after [drug-eluting stent (DES)] placement," Finn and colleagues said (JACC Cardiovascular Imaging, July 2008, Vol. 1:4, pp. 475-484).
Imaging morphology
There are a number of modalities in use today and several new methods on the horizon, Waxman said. Catheter-based imaging methods include intravascular ultrasound (IVUS) and now VH IVUS, which "analyzes the acoustic signature in vessels, which corresponds to different plaque morphologies," he said.
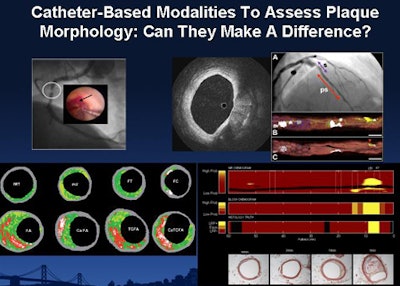 |
| Various catheter-based modalities used to assess plaque morphology before PCI include (clockwise from upper left) angioscopy, IVUS, near-infrared spectroscopy, and VH IVUS. |
"Coronary angioscopy is pretty much the grandfather of coronary imaging; you're looking for the yellow-reddish plaque that correlates with the lipid cores of the deep fibrous caps," he said. "Near-infrared spectroscopy provides us with chemograms, which maximize our ability to find a lipid-rich core."
Optical coherence tomography uses near-infrared light to visualize the vessel wall at the microscopic level, precisely measuring cellular lining thickness and gauging vessel response to deployed stents. Optical frequency domain imaging advances the technology with faster acquisition and real-time imaging, reducing motion artifacts and permitting the visualization and screening of larger tissue volumes.
MRI and especially CT offer excellent anatomic detail, which can help define plaque morphology alone or in combination with other modalities.
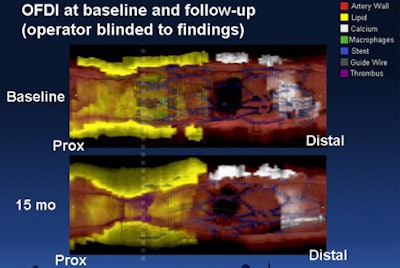 |
| Optical frequency domain imaging (OFDI) represents an advance over optical coherence tomography for evaluating plaque deposits in coronary arteries, offering faster image acquisition and wider fields-of-view. A blinded study at Waxman's institution used OFDI to study the history of vulnerable plaque over 15 months. Above, restenosis, thrombus, and progression of calcification can be seen compared to baseline image poststenting. Images courtesy of Dr. Guillermo Tearney, Ph.D., and Dr. Sergio Waxman. |
Morphology defines treatment response
In 2006, Ueda and colleagues reported that patients with multiple yellow plaques per vessel had a higher risk of suffering acute coronary syndrome events than those without the unstable plaques. Angioscopy revealed thrombus in 8% of bare metal stents and 42% of the drug-eluting stents at six months postprocedure.
"Thrombus occurred over drug-eluting stents at 64% of the yellow [unstable] plaques versus only 17% of white plaques," Waxman said. The authors recommended angioscopy to identify vulnerable patients prior to intervention (Journal of the American College of Cardiology, June 2006, Vol. 47:11, pp. 2194-2200).
Last year, Kubo and colleagues compared lesion morphologies after sirolimus-eluting stent implantation between patients with unstable angina and stable angina using optical coherence tomography.
At nine months' follow-up, the incidence of inadequately apposed stent (33% versus 4%, p = 0.012) and partially uncovered stent by neointima (72% versus 37%, p = 0.019) was significantly greater in the unstable angina patients compared to stable angina group, they wrote, concluding that optical coherence tomography found markedly different vascular response up to nine months after sirolimus-eluting stent implantation between the two patient groups.
"The studies raise a number of questions, such as whether the difference in outcomes due to plaque morphology is clinically relevant," Waxman said. Also at issue is whether the outcomes are improved sufficiently to justify the upfront costs and risks of imaging.
Will pre-PCI morphology assessment change patient management in terms of the size and type of stent selection, Waxman asked, or the duration of dual antiplatelet therapy? "Would we be able to select the stents based on morphology, for example -- a shorter stent in this patient and a longer one in this patient -- or use a different type of stent?"
Physicians at Waxman's institution have found a lot of room for improved management with morphology analysis, he said. A 52-year-old male who had received a bare-metal stent post-myocardial infarction presented with unstable angina and received a drug-eluting stent following the results of angiography. But he returned 15 months later with unstable angina.
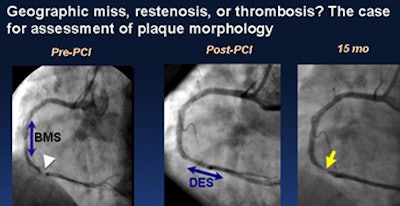 |
| A 52-year-old man with hypertension and dyslipidemia who received a bare-metal stent (BMS) to the right coronary artery after a myocardial infarction presented with unstable angina and underwent sirolimus-eluting stent (SES) implantation, but returned 15 months later with unstable angina, finally receiving a drug-eluting stent (DES) that was long enough to cover the vulnerable segment. |
"The stent was literally parked in the middle of a lipid-rich plaque, and at 15 months what we see is not only hyperplasia but growth of the necrotic core," Waxman said of the case. "These findings raise the question of whether [a different] stent could have prevented this."
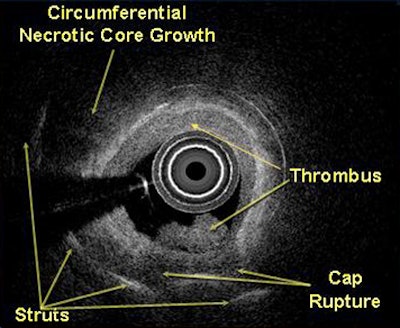 |
| IVUS study 15 months poststenting in a patient with thin-capped fibroatheroma shows noncalcified plaque growth, cap rupture, and propagating very late stent thrombosis. The case raises questions regarding how extending the stent beyond the necrotic core, using a bare-metal stent, or discontinuing dual antiplatelet therapy earlier, would have altered the healing process. |
Good answers to these questions will require more research and larger cohorts, but a lot is known from the studies already conducted, he said.
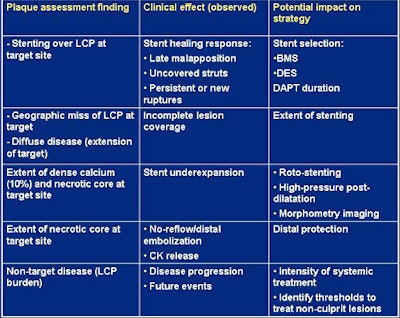 |
| Existing data from small studies and clinical reports of plaque morphology assessment before intervention show the potential impact on treatment strategies. |
In a study submitted for publication, Kubo and colleagues used VH IVUS to demonstrate the highly dynamic nature of nonculprit lesion progression in 99 patients and 216 lesions followed for 11 months, Waxman said.
Among 62 lesions with pathologic intimal thickening, 19% of the plaque area progressed to thick-capped fibroatheroma without calcification (ThCFA), and 10% progressed to thin-capped fibroatheroma (TCFA). Of 93 ThCFA lesions, 6% of the plaque area progressed to TCFA, 3% to fibrotic plaque, and 1% to fibrocalcific plaque. Among 20 TCFA, 65% of the plaque area progressed to ThCFA and 10% progressed to fibrotic plaque.
Determining appropriate thresholds for the treatment of nonculprit lesions will likely require multiple imaging modalities, Waxman said. Spot stenting may be acceptable in some cases, but more research is needed, he said.
Kim and colleagues found that plaque morphology can be used to predict stent underexpansion, Waxman said, and Park et al from Asian Medical Center in Seoul, Korea, found that necrotic core burden is associated with distal embolization.
"I've shown in various reports that certain findings are associated with certain effects," he said, adding that more research is needed to elucidate the role of imaging modalities and their effect on various treatment strategies.
"Plaque morphology is heterogeneous, which likely explains differences in response to treatment," he said. "Although cardiovascular procedural outcomes continue to improve, a one-size-fits-all approach to revascularization and prevention of events may hamper efforts to improve outcomes further."
Plaque morphology assessment with catheter-based imaging is showing promise in discriminating various treatment effects and directing strategies, he said. "However, evidence-based data regarding the clinical utility of morphologic assessment are lacking at present and should be a matter of further study."
Catheter-based plaque morphology assessment is likely to drive noninvasive imaging modalities to be used as tools prior to intervention and for screening and prevention of coronary artery disease, Waxman said.
By Eric Barnes
AuntMinnie.com staff writer
September 25, 2009
Related Reading
Primary PCI vs. prehospital lysis for MI: similar survival, August 19, 2009
Post-PCI eptifibatide infusion can be safely cut from 18 to 2 hours, March 12, 2009
Percutaneous cardiovascular procedures 'strikingly better' with radial access, March 10, 2009
CABG remains superior to PCI for severe coronary disease, February 19, 2009
MR angiography detects vascular changes during treatment for brain metastases, December 10, 2007
Copyright © 2009 AuntMinnie.com