"Translucent view" polyp rendering is inadequate for primary diagnosis in virtual colonoscopy (also known as CT colonography or CTC), but it can help distinguish adenomas from hyperplastic lesions and other likely benign findings, say researchers from Stony Brook University in Stony Brook, NY.
The proprietary technique used in virtual colonoscopy workstations (Viatronix, Stony Brook, NY) was highly sensitive for identifying adenomas, but it was low in specificity, according to preliminary study results.
"Translucent view is used to identify the internal structure of polyps that are identified on virtual colonoscopy," explained Thomas Santos at the 2010 International Symposium on Virtual Colonoscopy in Boston. The method uses a volume-rendering algorithm to view the images from an original 3D CT dataset. Co-authors on the paper describing the results included Joseph Marino and Matthew Barish, MD.
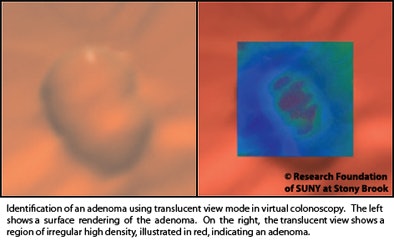 |
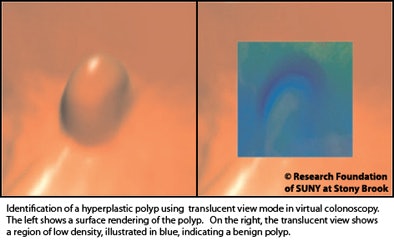
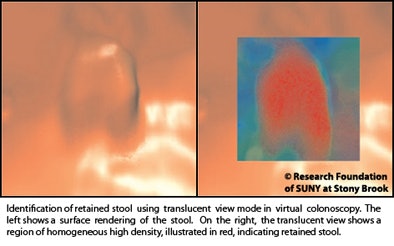
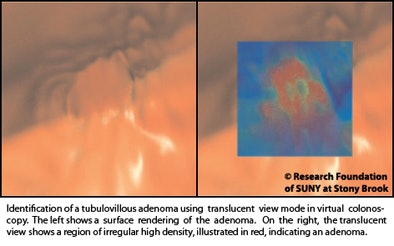
"Each voxel in the translucent view is assigned a specific color based on CT density from the original scan," Santos explained. High-density voxels, which have a higher likelihood of progressing to cancer, are rendered in red, low-density voxels in blue, and intermediate-density voxels in green, Santos said.
Once findings are identified, they are confirmed with the corresponding CT image. Using the technique, the researchers found, an experienced radiologist was able to determine whether or not a polyp was an adenoma approximately 77% of the time when both supine and prone views on virtual colonoscopy were considered.
 |
An experienced radiologist evaluated each polyp using the technique and scored it on a scale of one to five -- with a score of one corresponding to "definitely not an adenoma" and five corresponding to "definitely an adenoma," Santos explained.
"We score it first with the prone view, then with the supine view, and then ask [the reader] to make a total ranking after reading each view separately," he said.
From a total of 450 cases downloaded from the U.S. National Biomedical Imaging Archive (NBIA), the group analyzed 88 cases for the study because they had been referred to colonoscopy and polyps had been removed, providing histologic confirmation for each sample. A single experienced radiologist interpreted the results.
 |
Results using the radiologist's total score for each lesion (prone plus supine) yielded 52 true positives, 17 false positives, 15 true negatives, and four false negatives. Thus sensitivity was calculated at 93%, but specificity was only 47%, Santos said. Positive predictive value was 75%, negative predictive value was 79%, and accuracy was 77%.
"On the prone view, when the radiologist made a definitive diagnosis of adenoma [score = 5] or not an adenoma [score = 1], there was fairly high accuracy of 90%, and the midrange readings were significantly less accurate," Santos said. "But it's the 'indeterminate' diagnosis [score = 3] and 'probably an adenoma' [score = 4] categories that we're most worried about because these patients are going to have to be referred for optical colonoscopy."
 |
Of course, referrals from VC to colonoscopy are not made on translucent-view renderings alone, but if they had been based on this study, more than half of the study participants overall would have been referred to colonoscopy for a false-positive reading at VC, and more than one-third in the probable adenoma group would have been referred to colonoscopy based on a false-positive reading of the translucent view as well, Santos said.
Results for the supine view were similar to the prone in that "indeterminate" and "probably an adenoma" readings would often have been false positive at colonoscopy had they been referred.
On the plus side, using both supine and prone views, the radiologist was able to make a definitive diagnosis almost 50% of the time, compared with 40% using one view or the other, Santos said.
Using receiver operator characteristics (ROC) analysis, the area under the curve (AUC) was calculated for three scenarios: prone-only score, supine-only score, and total scores, yielding results of 0.7756, 0.7696, and 0.7983, respectively -- which did not yield a statistically significant difference.
"We decided that the diagnostic accuracy of 77% demonstrates that the translucent-view mode is inadequate at this time as a primary method of diagnosing polyp pathology," Santos said. "However, the high sensitivity of 93% suggests that this mode may show promise as an initial screening tool for adenomatous polyps."
The study team will soon expand the project to include more than 1,600 datasets from the NBIA database, and compare accuracy with and without the use of translucent view to determine its added utility. They will also incorporate more readers, including some inexperienced readers.
By Eric Barnes
AuntMinnie.com staff writer
December 7, 2010
Related Reading
VC may increase colon cancer screening, survey shows, November 10, 2010
Most choose VC over colonoscopy, study shows, August 27, 2009
Noncathartic bowel prep facilitates, complicates virtual colonoscopy, June 15, 2007
Group credits 3D reading for best-ever VC results, October 15, 2003
Copyright © 2010 AuntMinnie.com




















