Why do radiologists dismiss true-positive computer-aided detection (CAD) marks at virtual colonoscopy? Are there particular exam or polyp characteristics that lead to incorrect dismissals of CAD marks by radiologists? Researchers from London were eager to find out.
CAD is known to reduce the perceptual errors that pose the greatest challenge to correctly reading virtual colonoscopy (also known as CT colonography or CTC) exams, said Charlotte Robinson from University College London (UCL) in the U.K.
In some cases, standalone CAD has outperformed experienced radiologists, and CAD by itself quite often beats the performance of CAD as a second reader, once the radiologist has reviewed it. Because, unfortunately, radiologists sometimes dismiss true-positive CAD marks.
To learn more about this phenomenon, Robinson and colleagues Dr. Stuart Taylor and Dr. Steve Halligan initiated a study to identify why polyps correctly identified by CAD during CT colonography are incorrectly dismissed by radiologists, she said in a talk at the 2009 RSNA meeting.
The researchers examined 111 CAD-detected and colonoscopy-confirmed polyps 6 mm or larger from three previous studies that investigated radiologist performance with and without CAD -- using a total of 25 readers, Robinson noted.
Then, two experienced CTC readers who were blinded to the performance of the original 25 readers and the data reviewed each colonoscopy-confirmed lesion for numerous characteristics. They looked at everything from polyp size to morphology, location, tagging, relationship to folds, colonic curvature and wall thickness, and the total number of polyps and false-positive CAD marks in the dataset, she said.
Of the 111 polyps, the 86 polyps that were missed (i.e., unreported by one or more of the original readers) before the CAD software (Medicsight, London) was applied were divided into two groups: polyps that remained unreported after CAD ("no CAD gain," n = 36) and those that, after CAD, were reported correctly by at least one additional reader ("CAD gain," n = 50).
The two groups of findings -- representing "CAD gain" and "no CAD gain" -- were then compared to each other, and to a control group of the remaining 25 polyps that were detected by readers without CAD, using logistic-regression and Fisher's exact and Mann-Whitney tests.
Of the 111 polyps, 48 were sessile, 52 were pedunculated, a few were flat, and 22 were irregularly shaped, she said. CAD called about seven false positives per dataset.
Before application of CAD software, polyps 10 mm or larger that were deemed easy to visualize or uncoated by tagged fluid were less likely to be missed.
Control polyps (i.e., 100% detection pre-CAD application) were:
- More likely classified as easy to visualize (76%) than missed polyps (43%) (p < 0.001)
- Significantly larger than missed polyps (control polyp median size = 13 mm, missed polyp median size = 8 mm) (p = 0.003)
- Less likely to be coated or submerged by tagged fluid (40% of missed polyps versus 19% of control polyps) (p = 0.03)
After the application of CAD, the odds of a CAD detection benefit decreased with increasing polyp size (odds ratio = 0.92 [0.85, 1.00], p = 0.04) and irregular morphology (odds ratio = 0.28 [0.08, 0.92], p = 0.04).
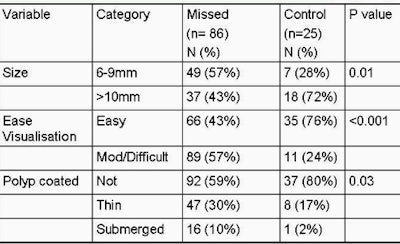 |
| Chart shows characteristics of "control" polyps (i.e., those found by radiologists pre-CAD) versus missed polyps. Control polyps were easier to visualize and larger than mixed polyps. Coated and submerged polyps were also more likely to be missed. All images courtesy of Dr. Stuart Taylor. |
Finally, polyps with overall irregular morphology that were also ≥ 10 mm comprised 11 of 36 (31%) "no CAD gain" polyps, but just three of 50 (6%) "CAD gain" polyps (p = 0.003).
Yet beyond these two features, no other polyp characteristic had any effect on CAD detection. Characteristics that did not affect CAD detection included:
- CAD mark placement
- Supine and/or prone visualization
- Number of CAD false positives
- Dataset quality
- Relationship to haustral fold
- Distension
- Colon wall thickness
- Diverticular disease
"The polyps for which CAD didn't benefit the reader might be irregular and bigger than 1 cm -- no other significant effect was seen by any other variable we scored," Robinson said.
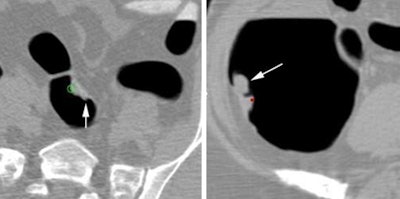 |
| At left, a 14-mm sigmoid polyp classified as irregular was missed by four of five readers before CAD, and no improvement was seen after CAD was applied. At right, an irregularly shaped 26-mm polyp in the ascending colon was missed by three of 10 readers, with no improvement after CAD. |
Among polyps larger than 6 mm, "those that were smaller, or coated, or submerged by fluid were at increased risk of getting missed by the unassisted reader," Robinson concluded. "However, after correct CAD prompting, larger lesions, particularly irregular in shape, were more prone to incorrect dismissal."
"Most radiologists know how to pick up the large lesions bigger than 1 cm, and we're relying on CAD to help determine the slightly more unusual irregularly shaped lesions, which we continue not to recognize," Robinson said.
More studies are needed to investigate the benefit of scrutinizing particularly difficult regions to ensure that true-positive CAD findings aren't dismissed, she said.
By Eric Barnes
AuntMinnie.com staff writer
January 14, 2010
Related Reading
VC CAD aids experts in detecting intermediate polyps, December 28, 2009
CAD catches most flat polyps on virtual colonoscopy, December 16, 2009
VC CAD nabs undetected polyps in jumbo screening study, October 29, 2009
Readers undaunted by VC CAD false positives, June 12, 2009
Virtual colonoscopy CAD improves flat-lesion detection, June 5, 2009
Copyright © 2010 AuntMinnie.com