
Multidetector-row CT is becoming a key player in many imaging tasks that were beyond the scope of single-slice CT. In the stomach, of course, the accuracy of the gastroscope remains beyond the reach of MDCT for imaging the subtlest mucosal lesions.
At the same time, MDCT's ability to assess the depth of invasion and gastric wall morphology has earned it growing acceptance in the staging and presurgical assessment of gastric cancer, replacing many x-ray barium studies in the process.
The principal question today is how to optimize CT gastrography, be it with 3D views, thinner slices, or -- in the case of two new studies in this month's American Journal of Roentgenology -- simple techniques that vastly improve distension, hence the diagnostic potential of CT gastrography.
In the first study, Japanese researchers used a water-filling method to improve detection of gastric cancer and evaluation of the extent of mucosal invasion (AJR, November 2005, Vol. 185:5, pp. 1,152-1,158).
In the second study, a team from Korea found that scanning patients in the left posterior oblique (LPO) position greatly improved distension and minimized residual fluid in the lower part of the stomach during CT gastrography (AJR, November 2005, Vol. 185:5, pp. 1,180-1,184).
Water distension
Seeking to determine whether water distension could improve the diagnosis of gastric cancers, Dr. Kensaku Shimizu, Dr. Katsunori Ito, and colleagues from the Yamaguchi Univesity School of Medicine in Japan examined 65 gastric cancer patients preoperatively with MDCT using the water-filling technique.
"Studies have indicated that the water-filling method with gastric CT allows clear depiction of the gastric wall and gastric tumor without overshooting artifacts by air in the lumen," the group wrote. "The combination of high-quality MPR (multiplanar reconstructions) with the water-filling method has the potential to improve diagnostic performance for detecting lesions and determining the depth of invasion of gastric carcinomas."
Pathologically proven gastric cancers were classified as pT1 (muscosal or submucosal invasion) in 34 patients, pT2 (muscle invasion) in 12 patients, pt3 (invasion of the serosa) in 9, and pT4 (invasion to adjacent organs or structures) in five patients.
Following a single-phase injection of 100 mL of nonionic contrast (2.8-3.0 mL/sec) and ingestion of 300-600 mL tap water just before imaging, all patients were imaged in the prone position (except for three in the supine position as their tumors were in the gastric fundus) on a multidetector-row Volume Zoom CT scanner (Siemens Medical Solutions, Erlangen, Germany).
Two-phase scanning (with a single breath-hold before each phase) was begun 30 and 80 seconds after contrast injection began, with data acquired at 4 x 1-mm collimation, reconstructed at 5 mm for abdominal screening and 1.25 mm (1-mm slice interval) in the stomach, with coronal and sagittal MPR images viewed on a workstation. Two experienced radiologists who were blinded to the clinical information reviewed each exam independently and resolved differences by consensus.
The overall detection rate for gastric cancers was 65%, including 96.2% (25/26) advanced cancers (pT2-pT4) and 41.2% (14/34) early cancers, the team reported. There was a statistically significant difference (p < 0.05) in the detection rate of early cancers between thin-slice MPR images and 5-mm axial slice images, but not between 5-mm axial images and 5-mm MPR images.
"In 34 early gastric cancers, thin-sliced MPR images depicted 68.8% of submucosal cancers ... and they showed 16.7% (3/18) of less invasive mucosal cancers," the researchers wrote. "The detection rate for grossly nonprotruding early cancers was comparatively low (28.6%)."
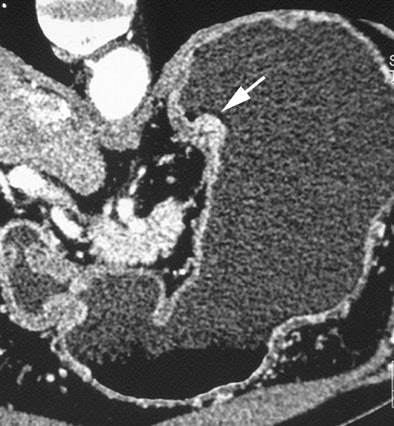 |
| Early gastric cancers. A 69-year-old man with protruding type of early gastric cancer. Oblique multiplanar reconstruction perpendicular to gastric wall shows protruding mass (arrow) of gastric cardia. Fig. 2A, Shimizu K, Ito K, Matsunaga N, Shimizu A, Kawakami Y. "Diagnosis of Gastric Cancer with MDCT Using the Water-Filling Method and Multiplanar Reconstruction: CT-Histologic Correlation" (AJR 2005; 185:1152-1158). |
The results were well-correlated with pathologic findings, and the overall accuracy of CT staging was 85%, they noted. On histology a high-attenuating abnormal inner layer corresponded to close proliferation of cancer cells, mainly mucosal and submucosal, whereas low-attenuating areas were indicative of scattered cancer cell diffusion such as in the proper muscle with dermoplastic changes and inflammatory reaction.
"In our seven early gastric cancers detected at MPR but not visible on 5-mm-slice axial images, six were located at the large or lesser curvature of the gastric angle or antrum," the group wrote. "Detection of early gastric cancers with 5-mm-slice axial images may be difficult because of partial volume artifacts where the gastric wall is tangent to the axial scan, such as the greater or lesser curvature of the gastric antrum or angle."
The accuracy of preoperative diagnosis is crucial for selecting patients for less-invasive laparoscopic surgery, they wrote.
"High-quality thin-sliced MPR using MDCT with the water-filling method has advantages in the reliable detection of advanced gastric cancers, acceptable evaluation of the depth of invasion of gastric carcinomas, and visualization of histologic changes … although there are some difficulties in the depiction of flat mucosal cancer and in accurate distinction between T2 and T3 tumors in some cases," they concluded.
Adjusting scan position
While the use of gastrointestinal 3D CT applications continues to grow, "the necessity for refining CT gastrography techniques has been unnoticed," according to Dr. Se Hyung Kim, Dr. Jeong Min Lee, and colleagues from Seoul National University and Chungnam National University in Korea.
The need did not go unnoticed by these researchers. "We hypothesized that performing CT gastrography with the patient in the left posterior oblique (LPO) position would provide better distension and less residual fluid for the lower part of the stomach than CT gastrography with the patient in the standard supine position," they wrote in their AJR study. "In previous 3D CT studies of the stomach performed with the patient in the supine or prone position, tumors located at the antrum were not well-delineated because of poor stomach distension or fluid retention."
After administration of 10 mg of hyoscine N-butylbromide (Buscopan, Boehringer Ingelheim, Ingelheim, Germany), two packets of orally administered effervescent granules with less than 5 mL water, and 70 seconds after injection of 120 mL of nonionic contrast media (iopromide, Ultravist, Schering, Berlin), the patients underwent imaging on a 16-slice MDCT scanner (Sensation 16, Siemens Medical Solutions, Erlangen, Germany) at 120 kVp, 100 effective mAs, 16 x 0.75-mm detector configuration, 15 mm/sec table feed (beam pitch 1.25) and 1-mm reconstruction with 30% overlapping sections.
For positioning, patients were randomly allocated into one of two groups, including 52 in the left lateral decubitus position "to shift the gastric contents from the lower two-thirds to the fundus of the stomach," then to the 30° LPO position "by placing a pillow at their back" for scanning. The remaining 33 patients were scanned in the standard supine position.
The results showed that the mean scores for gastric distension in most stomach segments were larger in the LPO patients than the supine group, and were statistically significant in the lower three segments, including the lower body, proximal antrum, and distal antrum (p < 0.004), but not statistically significant for the remaining three segments (p > 0.05).
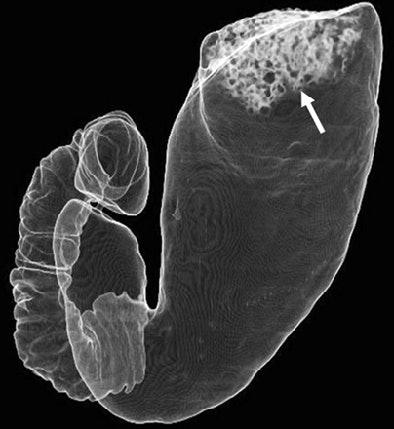 |
| CT gastrographic image of 64-year-old man in left posterior oblique (LPO) position. Transparent volume-rendering technique shows good distension of stomach except in gastric fundus. Note bubbly fluid (arrow, B) in fundus. Fig. 1B. Kim SE, Lee JM, Han JK, Lee JY, Shin KS, Choi IC. "Effect of Adjusted Positioning on Gastric Distention and Fluid Distribution During CT Gastrography" (AJR 2005; 185:1180-1184). |
LPO's advantage was even more pronounced in terms of residual fluid, with mean scores for the proximal and distal antrum together significantly larger among the LPO patients (p < 0.03) than the supine group. LPO trended higher for the remaining segments but the differences were not statistically significant (p > 0.05). The total score for both parameters in the LPO group was 3.6 ± 0.8 (mean ± SD) compared to 3.2 ± 1.0 for the supine group, and the difference was statistically significant (p < 0.0001).
"Unlike double-contrast barium studies in which imaging can be performed in multiple projections to allow the fluid to redistribute, scanning for CT gastrography should be limited to only one or two projections -- that is, the supine or LPO position and the right decubitus position," the authors wrote. "Positioning toward one's back in the LPO position just after turning onto one's left side can shift fluid in the gastric antrum to the gastric fundus, and subsequently allow a clean image of the lower gastric portion to be obtained."
Both axial and 3D images are needed to address the spectrum of gastric pathology, they added.
By Eric Barnes
AuntMinnie.com staff writer
November 14, 2005
Related Reading
Volumetric CT gastrography bests transverse scans for cancer staging, September 26, 2005
Preop chemoradiotherapy beneficial in resectable gastric cancer, July 29, 2004
Study reveals gender, ethnicity differences in esophageal, gastric cardia cancers, May 24, 2004
Extended lymph node dissection does not improve gastric cancer survival, April 4, 2004
Studies compare, optimize contrast in the abdomen, June 28, 2004
Copyright © 2005 AuntMinnie.com




















