A new digital subtraction technique improves the delineation of lesions in MR colonography, researchers at the University of Essen in Germany concluded in a preliminary study.
"The dark-lumen approach (to MRC) is cost-effective because you mainly use just water to render the colonic lumen dark," said lead investigator Dr. Christoph Herborn in a presentation at the 2004 European Congress of Radiology in Vienna. "The technique has also been optimized by the use of spasmolytic agents...and since you acquire both plain and contrast-enhanced data, (dark-lumen MRC) seems suitable for a subtraction technique as we know it from digital subtraction angiography."
By subtracting the plain from the contrast-enhanced MR colonography data, the researchers hoped to improve the visualization of colonic wall lesions as a result of their focal uptake of contrast, Herborn said.
The group examined 12 male patients (mean age 56.4 years) and eight female patients (mean age 54.1 years) with suspected colonic polyps. Twelve hours before the exam the patients ingested 3L of a polyethylene glycol solution for colonic cleansing.
Immediately before imaging, the patients also received a body-weight-adjusted dose of approximately butylscopalamine (Buscopan) intravenously to stop peristaltic action, and the colon was filled with 1.5 to 3L of water at body temperature. The patients also received an intravenous injection of 0.2 mmol/kg Gd-BOPTA as a contrast agent (Multihance, Bracco, Milan, Italy), approximately 75 seconds before scanning was initiated.
The patients were imaged in the prone position only on a 1.5-tesla scanner (Magnetom Sonata, Siemens Medical Solutions, Erlangen, Germany) equipped with a phased-array surface coil.
TrueFISP images were acquired to document the filling of the colon, followed by the "heart" of the protocol, a 3D VIBE (3D T1-weighted GRE) sequence acquired in the coronal plane over 24 seconds in a single breathhold, Herborn said.
- TrueFISP images were acquired at TR/TE 2.4/1.2 ms, FA 60º, slice thickness 5 mm.
- 3D VIBE images were acquired in the coronal plane at TR/TE 3.1/1.1 ms, FA 12º, FOV 400 x 400 mm, matrix 168 x 256, effective slice thickness 4.0 mm.
"We performed three acquisitions...and simply subtracted the native data from the contrast-enhanced scan," Herborn said.
The images were reviewed on a postprocessing workstation (Leonardo, Siemens) by two radiologists blinded to all results. The readers looked for colorectal pathology, and assessed the value of the subtracted dataset for lesion depiction in each exam, rating it on a five-point Likert scale from 1 ("very helpful") to 5 ("very unhelpful"). Finally, all of imaging results were compared with a previous endoscopic exam.
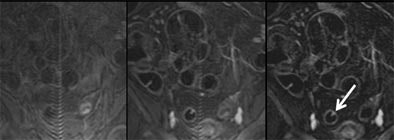 |
| Three views of the colon in a 48-year-old patient with a single polyp are seen at different time points: 1) without contrast material (left); and 2) following intravenous injection of 0.2 mmol/kg Gd-DOTA (Dotarem). This view shows good uptake of contrast material to the colon wall, and especially to the polyp (middle). Image at right 3) shows subtraction of the plain from the enhanced image, providing optimal visualization of regions with contrast uptake. Residual stool has also been subtracted, rendering the colonic lumen homogeneously dark. Images courtesy of Dr. Christoph Herborn. |
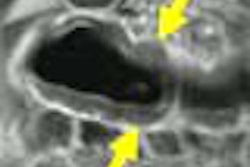
"Here is a patient with colon cancer," Herborn said, showing a digitally subtracted image. "You can nicely see this large mass here in the distal portion of the sigmoid colon. This patient also suffers from a liver metastasis, which points to the inherent additional information you can get from cross-sectional images compared to endoscopy."
According to the results, focal uptake of contrast was easily detectable using the dark-lumen MR colonography technique with digital subtraction.
The group detected a total of three polyps (8 mm to 14 mm), two inflammatory lesions, and one carcinoma among eight patients. MRC missed two small polyps (3 mm and 4 mm) that were found in conventional colonoscopy.
The overall sensitivity and specificity of dark-lumen MRC for the detection of colorectal lesions were 67% and 100%, respectively, without digital subtraction, and 80% and 100%, respectively, with digital subtraction. A single 5-mm polyp not seen in the unsubtracted data was detected following digital subtraction, Herborn said. The radiologists rated the digital subtraction dataset "helpful," with a mean value of 1.8.
"I'd like to conclude from this preliminary study that the subtraction of plain from contrast-enhanced MR colonography datasets seems to be a beneficial supplement, since you already have the data," Herborn said. No additional scanning or expense is required to use the technique, he said; simply postprocessing on the computer.
An audience member asked if his group's digital subtraction technique posed the same problem with artifacts as it does in digital subtraction angiography. Herborn said he has seen only very minor partial-volume artifacts so far, but that the group is keeping an eye out for them.
"We've looked at different imaging modalities like endoscopy, CT, or MRC for detection and delineation of the disease," Herborn said. "At least in our institution ... we found that due to excellent soft-tissue contrast and the good spatial as well as temporal resolution, MR is the way to go with regard to colon exams. Since there is no radiation going into the examination, it's most favorable for screening purposes."
By Eric BarnesAuntMinnie.com staff writer
July 21, 2004
Related Reading
New tagging, subtraction techniques aim for better compliance in VC, March 8, 2004
German group optimizes barium-sulfate tagging in MR colonography, January 22, 2003
Copyright © 2004 AuntMinnie.com