On July 5 the World Health Organization removed Taiwan, China, from its list of areas with recent local transmission of severe acute respiratory syndrome (SARS). Taiwan’s delisting follows that of Toronto, Canada, three days earlier, and marks the last area to be removed from the list.
For now, the absence of new SARS cases since June 15 has brought hope around the world, and a return to normal life in areas hardest hit by a virus that claimed 8,439 victims and 812 lives in the first half of 2003. In many patients lucky enough to survive the initial infection, however, a new study from Hong Kong confirms early indications that SARS has left a debilitating trail of lung abnormalities.
In a study published online in Radiology, Dr. Gregory Antonio, Dr. K.T. Wong, Dr. David S.C. Hui, and colleagues from the Prince of Wales Hospital in Hong Kong examined 24 SARS patients (10 men, 14 women, ages 23-70, mean age 39) following their discharge from the hospital. With the aid of thin-section CT, they found parenchymal abnormalities in 96% of 24 patients who remained symptomatic.
"Although these patients met the discharge criteria and were otherwise well enough to perform their daily activities, they complained of exertional dyspnea and/or reduced exercise tolerance at clinical follow-up," Antonio and colleagues wrote. "Because this was a new entity with no previous literature about disease progression for guidance, we performed thin-section CT (in addition to conventional chest radiography) in the patients to document any residual lung abnormalities. An additional 19 patients met our criteria but were not included in our study since thin-section CT, which had been scheduled, had not yet been performed" (Radiology, June 12, 2003, 10.1148/radiol.2283030726).
Imaging, including chest x-ray and CT, was performed an average of 36.5 days after hospital admission (range 16-56 days), and an average of 17.8 days (range 1-33 days) after discharge, Antonio and colleagues wrote. Nine of the patients underwent CT upon admission.
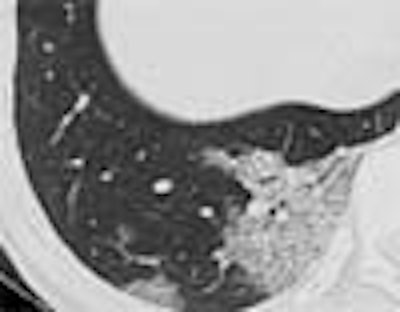
 |
| Transverse thin-section CT scan of right lower lobe in a 25-year-old woman with SARS (obtained at day 3 after admission) shows two areas of ground-glass opacification, with thickened interlobular septa giving crazy-paving appearance. Images and caption from Radiology Online, June 12, 2003, republished by permission of the author and the Radiological Society of North America, © RSNA 2003. |
All CT images were obtained on a HiSpeed Advantage scanner (GE Medical Systems, Waukesha, WI) using 1-mm slice thickness with a 6-mm gap, supine positioning, scanning during inspiration, 120 kVp, 140 mAs.
Three radiologists reviewed each lobe in the dataset on a viewing console, assessing each abnormality with the aid of a zoom function, and establishing their findings by consensus. The images were reviewed for ground-glass opacification, characterized by increased attenuation of the lung parenchyma that did not obscure the underlying vasculature. The images were also examined for interstitial thickening, airspace consolidation, bronchiectasis, and architectural distortion. The radiologists also looked for the presence of nodules or masses, cavitation, calcification, and emphysema.
"The presence of parenchymal bands, irregular interfaces (bronchovascular, pleural, or mediastinal), and traction bronchiectasis were considered as evidence of fibrosis," the authors wrote. "Thickened interstitium could not be used as evidence of fibrosis since it may also be present during the acute illness."
Four chest x-rays were also obtained in each patient during the course of care, and were evaluated in a manner similar to the CT exams. Chest radiography was abnormal in 20 of 24 patients at discharge.
In CT there were 15 patients (62%) (eight men, seven women, mean age 45) with evidence of fibrosis, designated as Group 1. There were nine patients (two men, seven women, mean age 30.3 years) without evidence of fibrosis, designated as Group 2.
CT was abnormal in 23 of 24 patients; all 23 had ground-glass opacification, and septal thickening of the intralobular septa and intralobular interstitium, Antonio and colleagues wrote. In all, 15 of 24 patients (62%) had evidence of fibrosis. Eight of nine patients who underwent CT upon admission to the hospital had residual ground-glass opacification and thickened interlobular septa. Of these, eight showed improvement in follow-up CT, while the 9th patient had complete resolution of lung abnormalities.
The 15 patients with evidence of fibrosis (Group 1) stayed in the hospital longer than Group 2 patients (22.3 vs. 16.4 days). More Group 1 patients were also admitted to intensive care, and Group 1 also had higher peak lactate dehydrogenase levels (438.9 vs. 355.6 U/L) compared to Group 2. Group 1 patients needed more doses of pulsed intravenous prednisone than Group 2 patients. Finally, more abnormal lung segments were seen in CT follow-up of Group 1 patients (mean 10.8 vs. 4.7 for Group 2).
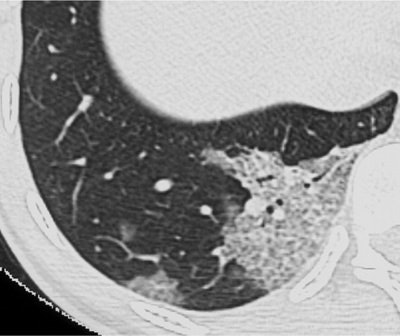
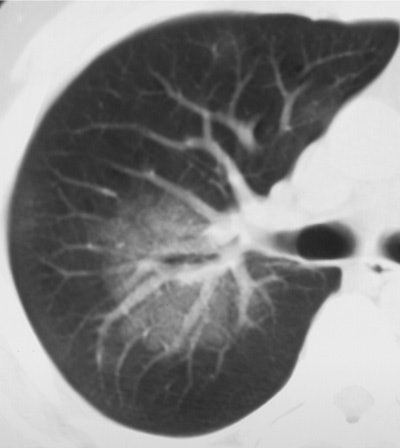 |
| Above (Fig. 2a), transverse conventional CT scan in 33-year-old man with SARS (obtained at day 4 after admission) shows ground-glass opacification. Below (Fig. 2b) follow-up thin-section CT scan (obtained at day 46 after admission, 29 days since discharge) of the corresponding area shows evidence of fibrosis, such as parenchymal bands, irregular interface, and traction bronchiectasis. Images and captions from Radiology Online, June 12, 2003, republished by permission of the author and the Radiological Society of North America, © RSNA 2003. |
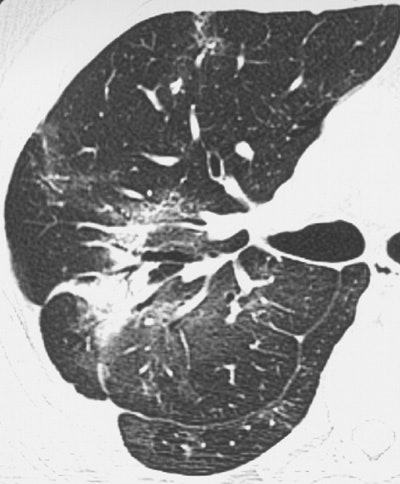 |
Of 317 patients admitted to the authors' institution for SARS (based on WHO criteria) 55 remained in the hospital, 35 died, and 227 were discharged, the authors wrote. Forty-three patients who were discharged had reduced tolerance for exercise.
"In our study, follow-up thin-section CT scans obtained in the discharged patients have shown that fibrosis occurred in more than half (62%) of patients," the authors wrote. "Findings of this study have also revealed how rapidly (mean follow-up, 36.5 days after hospital admission and 17.8 days after discharge) fibrosis may begin in patients with SARS. Viral pneumonia usually resolves without any clinical and radiologic sequelae."
The fact that all nine patients imaged with CT at admission improved at follow-up suggests that the initial lung parenchymal changes are inflammatory, and may be amenable to therapy, according to the authors. The hospital is currently experimenting with corticosteroids and other steroid-sparing immunomodulating agents to head off potentially reversible components of SARS-induced fibrosis, they wrote.
"This damage may be related to the proposed pathogenesis of lung damage by exaggerated cell-mediated host immune response elicited by a viral antigen," the authors wrote. "We believe the presence of pulmonary fibrosis would at least partially account for the patients' symptoms."
More follow-up time will be needed to determine the extent to which the parenchymal changes will resolve in the future, the authors wrote, noting that areas of severe architectural distortion seem likely to remain.
By Eric BarnesAuntMinnie.com staff writer
July 7, 2003
Related Reading
Chest CT useful in diagnosing questionable SARS cases, May 21, 2003
SARS presents distinct radiological patterns, May 6, 2003
Lung scarring found in Hong Kong SARS victims, May 2, 2002
Guideline advises on management of SARS, April 9, 2003
China seals hospital over SARS, Canada angry at WHO, April 24, 2003
Copyright © 2003 AuntMinnie.com




















