American radiology residents reported on clinical rotations in Nepal during which they used point-of-care ultrasound (POCUS) for high-risk pregnancies in a commentary published January 30 in the Journal of the American College of Radiology.
Researchers led by Rebecca Ward, MD, from the University of Pennsylvania in Philadelphia, highlighted that the residents’ time working with Nepalese sonographers was successful in imaging women in rural areas within the country, aiding in the fight against maternal mortality.
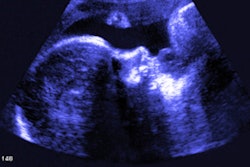
“With a small handheld portable probe and a tablet or phone, a provider can identify a range of life-threatening conditions,” Ward and co-authors wrote. “Even the limited ultrasound examinations performed at the point of care can provide information which may be used to triage patients and facilitate transportation to specialized centers when necessary.”
Increased maternal mortality rates have been linked to several factors, including limited access to healthcare, poor nutrition, and inadequate hygiene measures, along with high-risk pregnancies due to placental and fetal abnormalities.
Previous research suggests that POCUS can help with access to healthcare by being used in geographic areas that don’t have easy access to medical facilities. Its use among non-physicians has also been explored. In Nepal, where about 75% of the nation is classified as rural, adequate pregnancy screening can be hard to come by. The researchers also noted that Nepal has a shortage of physicians.
Ward and colleagues described the experience of American radiology residents in two Nepalese clinics.
In the first clinic, the residents worked with an existing POCUS team in a pregnancy ultrasound clinic in the Mahalaxmi municipality on the outskirts of Kathmandu. They scanned 25 women ranging from five to 39 weeks in pregnancy with a portable, curved probe. The collaboration found several high-risk pregnancy features within the women. These included polyhydramnios, subchorionic hemorrhage, low fetal heart rate, and placenta previa. The scanned women were informed of the findings and referred to the obstetrics department of a nearby hospital.
The second outreach clinic was located about two hours east of Kathmandu. Here, 15 women ranging from the first through third trimester of pregnancy presented to the clinic. Of the total women, one was identified with oligohydramnios, and another was diagnosed with low fetal heart rate. These women were referred to the nearest hospital for further testing and management.
The Ward team highlighted that the residents’ experience in Nepal added to their POCUS exam and interpretation skills by having them work with limited clinical information and no additional imaging modalities. They added that the residents took the opportunity to “witness the cultural and economic intersections of imaging, notably the value of imaging in caring for the most underprivileged in society.”
Based on these results, the report authors encouraged radiology residents to hone their skills with POCUS when working in global medicine and health equity initiatives.
“Further, radiology residencies should consider providing radiology residents ample time to learn the art of ultrasound scanning and POCUS,” they wrote.
The full report can be found here.