3D-printed radioprotective shields produced from CT images can be used to protect healthy structures in the gastrointestinal tract during radiation therapy procedures, according to research published online April 27 in Advanced Science.
In an initial proof-of-concept study, a multi-institutional and multidisciplinary team from Brigham and Women's Hospital, Dana-Farber Cancer Institute, Massachusetts General Hospital (MGH), and the Massachusetts Institute of Technology developed 3D-printed shields that successfully protected healthy tissue in rats and pigs. The group also estimated that the shields could reduce radiation in areas of the mouth by 30% in head and neck cancer patients and in the gastrointestinal tract by 15% in prostate cancer patients -- while being more cost-effective than a hydrogel rectal spacer.
"Our results support the feasibility of personalized devices for reducing the side effects of radiation therapy," said first author Dr. James Byrne, PhD, in a statement from Brigham and Women's Hospital. "This personalized approach could be applicable to a variety of cancers and holds the potential to reduce the burden of radiation injury and toxicity for our patients."
Radiation therapy can damage healthy tissue, including tissue in the mouth and gastrointestinal tract. These tissue injuries can lead to oral mucositis, esophagitis, and proctitis, and over 200,000 patients in the U.S. are estimated to experience gastrointestinal-related injuries caused by radiation damage to normal tissue, according to the researchers.
As a result, Byrne and colleagues sought to develop a personalized solution for protecting patients. After testing a range of solid and liquid materials for the radioprotective shields, they settled on materials with high atomic numbers to block gamma and x-rays, as well as other materials to reduce radiation backscatter.
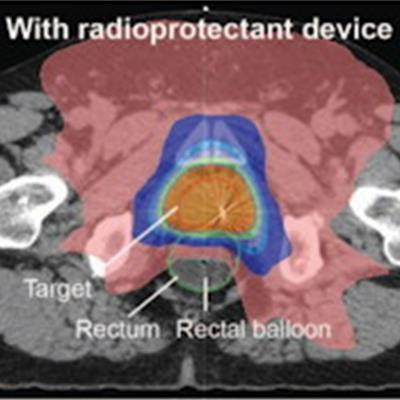
Using the open-source 3D Slicer software application, the organs at risk for radiation-induced damage are contoured on diagnostic CT scans. These contours are then generated into 3D models. Next, the personalized radioprotective shields are 3D-printed with incorporated attenuating materials to fit the 3D models, according to the researchers.
In initial testing on rats and pigs, the team found that the devices could protect healthy tissue in the mouth and rectum in rats and were feasible and reproducible in pigs. In human simulation studies, dosimetric modeling in three oral cavity cancer patients showed a 30% dose reduction to the normal buccal mucosa and a 15.2% dose reduction in the rectum for prostate cancer when the radioprotectant material was in place, according to the investigators.
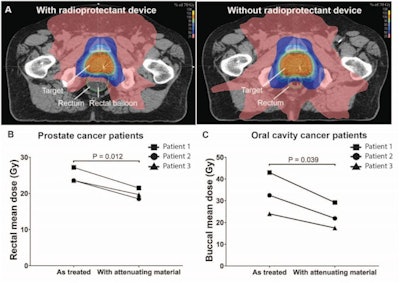 Dosimetric modeling of radioprotectant devices in patients. (A) Axial CT images of radiation plan of a prostate cancer patient with a radioprotectant device compared to without a radioprotectant device (as treated) showcasing the impact of the device on reducing radiation exposure to the rectum. Comparison of dosimetric plan with or without attenuating material in (B) prostate cancer patients (n = 3) and (C) oral cavity cancer patients (n = 3). Mean doses were calculated as the average of the dose to each voxel contained within the organ; voxels of 2 mm × 2 mm in X and Y, and 2.5 mm in the Z direction; p-value was determined by paired two-sample t test. Images and caption courtesy of Advanced Science and Dr. James Byrne, PhD, et al. Licensed under CC BY-SA 4.0.
Dosimetric modeling of radioprotectant devices in patients. (A) Axial CT images of radiation plan of a prostate cancer patient with a radioprotectant device compared to without a radioprotectant device (as treated) showcasing the impact of the device on reducing radiation exposure to the rectum. Comparison of dosimetric plan with or without attenuating material in (B) prostate cancer patients (n = 3) and (C) oral cavity cancer patients (n = 3). Mean doses were calculated as the average of the dose to each voxel contained within the organ; voxels of 2 mm × 2 mm in X and Y, and 2.5 mm in the Z direction; p-value was determined by paired two-sample t test. Images and caption courtesy of Advanced Science and Dr. James Byrne, PhD, et al. Licensed under CC BY-SA 4.0.After performing cost-effectiveness analysis for use in localized prostate cancer radiotherapy, the study authors also found that the 3D-printed device was more effective and less costly than a strategy in which no protective devices were used, and it would be more cost-effective than a hydrogel rectal spacer.
"These devices have the potential to shift the paradigm of clinical management of patients receiving radiation therapy for cancer; by reducing radiation‐associated morbidity and therefore improving treatment adherence, they have the potential to improve survival," Byrne et al wrote.
But they noted that more work will be needed before this approach is ready for clinical use.
"However, these data suggest personalized 3D‐printed radioprotectant devices may have great potential to reduce radiation toxicity in clinical settings where radiation is used, including neoadjuvant and adjuvant therapy, curative treatment, and palliative treatments," they wrote. "This personalized approach could be applicable to a variety of cancers that respond to radiation therapy, including head and neck, lung, prostate, anal, skin, and gynecological cancers, sarcomas, and lymphomas."