Requiring radiation oncologists to obtain prior authorization from third-party entities before starting cancer therapy is causing unnecessary delays and potentially life-threatening outcomes for patients, according to a survey released April 25 from the American Society for Radiation Oncology (ASTRO).
A poll of 673 ASTRO members found that 30% of radiation oncologists said waiting for prior authorization approval caused treatment delays of one to three days, while 32% of the respondents said they had to put off therapy for four to five days.
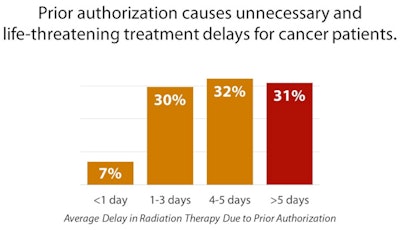 Prior authorization can cause delays in patient treatment, according to results of an ASTRO survey. Image courtesy of ASTRO.
Prior authorization can cause delays in patient treatment, according to results of an ASTRO survey. Image courtesy of ASTRO.And each day of delayed treatment increases a cancer patient's risk of mortality.
"What is unconscionable is that one-third of the physicians found that the delays were greater than five days. In many experiences, they had patients whose treatments were delayed in excess of two weeks," said Dr. Vivek Kavadi, vice chair of ASTRO's payor relations subcommittee and a radiation oncologist at Texas Oncology. "Not only does prior authorization cause unnecessary delays, but these delays are potentially life-threatening for cancer patients."
What's the point?
More than 1.7 million people in the U.S. will be diagnosed with cancer this year, and approximately 1 million of them will receive radiation therapy. Naturally, in cancer care, timely treatment matters. Yet restrictive prior authorization practices are delaying patients from receiving lifesaving therapies, radiation oncologists stress.
Prior authorization was designed to ensure that patients receive the most appropriate and efficacious treatment possible for their conditions and to prevent the overutilization of services. Whether the process is accomplishing those goals is up for debate, since 62% of respondents to the ASTRO survey said that most of their prior authorization denials were overturned on appeal. That statistic alone "raises serious questions about the justification of the denial in the first place," Kavadi said.
 Dr. Paul Harari, from the University of Wisconsin-Madison.
Dr. Paul Harari, from the University of Wisconsin-Madison.The prior authorization system was intended as "a path to strengthen American healthcare," said Dr. Paul Harari, ASTRO board chair and chairman of human oncology at the University of Wisconsin-Madison (UWM). "In its current form, however, it is causing unnecessary harm, anxiety, and delays in treatment for cancer patients."
At UWM's Carbone Cancer Center, there are "15 busy radiation oncologists," Harari added. "The challenges they face in the delays associated with prior authorization are a constant cause of concern. We very rarely have a case denied following prior peer-to-peer review or appeal. However, the many hours spent by our physician providers and the delays in commencing treatment for these cancer patients can never be recovered."
Delays in treatment certainly can have an adverse effect on a cancer patient's outcome. A report from the Cleveland Clinic concluded each week of delay in beginning cancer therapy increases a patient's risk of mortality by 1.2% to 3.2%.
Reinventing the wheel
Many radiation oncologists also must feel like they are spinning their wheels when they seek third-party approval for tried-and-true treatments. Kavadi cited the example of rectal cancer, in which the combination of radiation and chemotherapy before surgery has been a well-established practice since the 1980s.
 Dr. Vivek Kavadi, from Texas Oncology.
Dr. Vivek Kavadi, from Texas Oncology."If that's the case, why in 2019, when I see a patient with rectal cancer, do I have to fill out a prior authorization form to give the standard optimum treatment?" he countered. "These are the types of nuisances that doctors have to deal with. It is appropriate to question things that are unusual or something that is very expensive if alternative treatments are available, but to question everything is not reasonable and appropriate, and it does not add any value."
Part of the problem could be due to inadequate review of patient treatment plans. According to 44% of ASTRO respondents, between 76% and 100% of their care strategies were not peer-reviewed with another licensed radiation oncologist. In addition, radiation oncology benefit management (ROBM) companies required 85% of radiation oncologists to submit multiple treatment plans at some point during the review process. That demand simply adds more paperwork to already overwhelmed physicians.
AMA concurrence
The American Medical Association (AMA) conducted a similar survey of some 1,000 members last year, which described the prior authorization process as "plagued with administrative waste and lacking consistency and transparency," said Dr. Bruce Scott, an otolaryngologist and a member of the AMA's board of trustees. "The very manual, time-consuming process used in these programs diverts valuable resources away from direct patient care."
 Dr. Bruce Scott, from the AMA's board of trustees.
Dr. Bruce Scott, from the AMA's board of trustees.The AMA survey revealed that each week a medical practice completes an average of 31 prior authorization requirements per physician, which consumed a weekly average of 14.9 hours of physician and staff time. To keep up with the paperwork, 36% of AMA physicians employ staff who work exclusively on tasks associated with prior authorization, which in turn diverts funds from patient care.
"But the problem goes much deeper than physician frustration and wasted resources," Scott added. "It results in delays of treatment, it adds stress for our patients, and it is simply bad medicine."
That stress and anxiety associated with prior authorization delays prompted patients to "sometimes" or "often" abandon their recommended course of treatment, according to 73% of AMA physicians. In addition, 28% of the respondents reported that prior authorization requirements for drugs, tests, and treatments have led to serious or life-threatening events for their patients, which included hospitalization, death, disability, or permanent bodily damage.
Solutions anyone?
To alleviate the prior authorization grind, the AMA joined with the American Hospital Association, American Pharmacists Association, Medical Group Management Association, as well as the Blue Cross Blue Shield Association and health insurers trade group America's Health Insurance Plans in January 2018 to adopt five key principles for industrywide improvements. They include the following:
- The selective application of prior authorization
- A prior authorization review and volume adjustment
- The improvement of transparency and communication of prior authorization
- Automation to improve transparency and efficiency
- The continuity of patient care
"Unfortunately, the experience of physicians since then indicates that most health plans are not making meaningful progress in implementing each of the five areas of prior authorization reform as agreed to in the January 2018 consensus statement," Scott said.
Both ASTRO and the AMA have advocated for prior authorization reform with elected national and state representatives and have worked with various ROBMs to simplify the process, but there remains much room for improvement and compromise.
"There is no question that the criticality of cancer care being afforded to patients who require effective and rapid treatment is a national imperative," Harari said. "Cancer patients deserve to have high-quality care, and they do not deserve to have unwarranted delays in treatment, particularly when that has an adverse impact on their likelihood of care and survival."
Other ASTRO survey results include the following:
- 73% of respondents said their patients regularly express concern to them about the delay caused by prior authorization.
- 17% of radiation oncologists said they lose more than 10% of time that they could be caring for their patients focused instead on dealing with prior authorization issues.
- 39% of radiation oncologists spend 5% to 10% of their average workday on prior authorization.
- 37% of radiation oncologists needed prior authorization for at least a quarter of their cases.