Researchers are reporting early success with a novel quantitative MRI technique designed to calculate changes in tissue volume within the prostate to improve the diagnosis of cancer and better evaluate its aggressiveness, according to a study published in the June issue of Radiology.
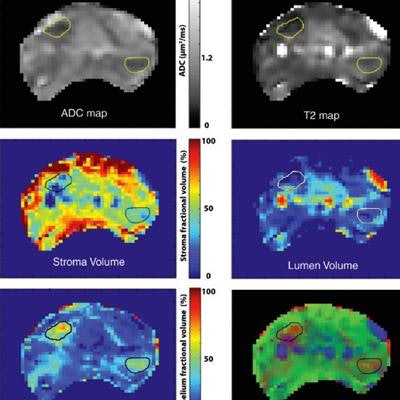
The three-part MR technique targets the epithelium, lumen, and stroma, which are known to change size with the presence of cancer. By quantifying differences in volume fraction, apparent diffusion coefficient (ADC) value, and T2 value between cancerous and normal tissue, the researchers were better able to assess patients' conditions.
"We are very excited about this tool because it gives us a virtual pathology whereby we can get information that we only could get after biopsy or prostatectomy," said co-author Dr. Aytekin Oto, a professor of radiology and surgery at the University of Chicago.
MRI's limitations
While MRI has become an important tool to diagnose suspected cases of prostate cancer and help patients avoid unnecessary biopsies, the modality has some shortcomings that limit its applicability to a wider patient population.
 Dr. Aytekin Oto from the University of Chicago.
Dr. Aytekin Oto from the University of Chicago."The most important limitation is the lack of reproducibility of results," Oto told AuntMinnie.com. "The interpretation of prostate MRI is currently based on subjective evaluation of multiple sequences, and there is an overwhelming amount of information to be handled by a radiologist."
A second challenge, he added, is that despite recent technical advances, MRI can still miss 20% to 30% of clinically significant prostate cancers. The omissions are primarily due to similarities with normal glands and benign conditions. A third limitation ties into the increasing use of prostate MRI for targeted biopsies, which boosts the number of false positives on MRI.
"The whole point of using MRI before biopsy is to diminish the number of biopsies that need to be done, but by picking all these false-positive areas, we are actually contributing to the problem of unnecessary biopsies," said Oto, who also serves as section head for abdominal imaging. "It is because of these three reasons that we believe there is a clear need to improve prostate MRI and make it available to a larger patient population."
Hybrid multidimensional MRI measures changes in ADC and T2 and uses these changes "as a source of information about the underlying tissue microstructure," the study authors wrote. "As a result, hybrid multidimensional MRI could provide quantitative estimates of tissue composition by exploiting the coupled T2 and ADC values associated with each tissue component."
Prostate targets
The researchers targeted a specific trio of structures: the epithelium, lumen, and stroma. Previous studies had shown that the epithelium's volume increases with cancer, compared with a normal or benign prostate, while lumen and stromal volumes decrease when the disease is present. These changes, however, had yet to be quantified noninvasively.
"We wanted to explore this pathological characterization of prostate cancer and come up with some tissue estimates ... based on quantitative MRI," Oto said. "We believe that these changes are on a scale that we can capture by using special MRI techniques. That is how this new hybrid MRI protocol was developed."
For the study, the researchers prospectively recruited 22 consecutive patients between March 2012 and December 2016. The subjects had biopsy-proven prostate cancer and elevated levels of prostate-specific antigen (PSA), and they were scheduled to undergo radical prostatectomy (Radiology, June 2018, Vol. 287:3, pp. 864-873).
Prior to surgery, the men underwent multiparametric MRI on a 3-tesla scanner (Achieva, Philips Healthcare) with a six-channel cardiac phased-array coil placed around the pelvis and an endorectal coil.
The researchers found a total of 28 tumor regions of interest (ROIs): 11 lesions were classified as Gleason score 3+3, 11 as Gleason score 3+4, three as Gleason score 4+3, and three as Gleason score 4+5. There were also 71 normal tissue ROIs: 20 were in the peripheral zone, 19 in the transition zone, 17 in the central zone, and 15 in the anterior fibromuscular stroma.
Oto and colleagues estimated volume fractions, ADC values, and T2 values of the three areas based on their diffusion and T2 relaxation properties. Tissue component volumes were then calculated on a voxel-by-voxel basis. A receiver operating characteristic (ROC) analysis was also performed to assess the parameters for differentiating prostate cancer from benign tissue.
Distinguishing disease
The results confirmed that prostate cancer results in significantly increased fractional volumes of the epithelium, while fractional volumes of the lumen and stroma were reduced. While ADC and T2 values were lower in cases of prostate cancer, the differences were not statistically significant as compared with normal prostate tissue.
| Mean volume fractions for prostate cancer and normal tissue | |||
| Cancer | Normal tissue | p-value* | |
| Epithelium | 48.8% ± 9.2% | 23.2% ± 7.1% | 0.0001 |
| Lumen | 14.0% ± 5.2% | 26.4% ± 14.1% | 0.040 |
| Stroma | 37.2% ± 9.1% | 50.5% ± 15.7% | 0.020 |
| ADC, T2 values for prostate cancer and normal tissue | |||
| Cancer | Normal tissue | p-value* | |
| ADC | 0.86 ± 0.18 µm2/msec | 1.34 ± 0.24 µm2/msec | 0.102 |
| T2 | 76.3 ± 22.9 msec | 104.2 ± 47.1 msec | 0.123 |
"ROC analysis showed that increased epithelium and reduced lumen volume are very effective markers for the diagnosis of prostate cancer," the authors wrote. "The area under the ROC curve for differentiation of cancer from normal prostate was highest for fractional volume of epithelium (0.991), followed by fractional volumes of lumen (0.800) and stroma (0.789)."
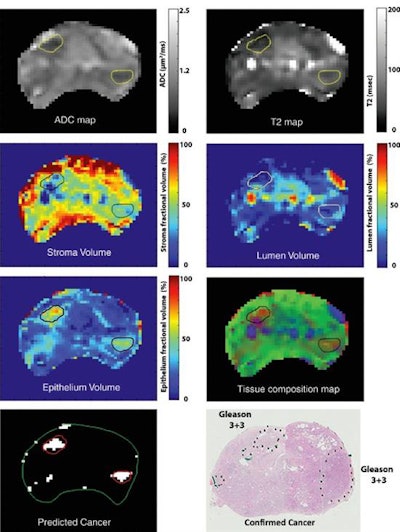 Tissue composition maps for the stroma, epithelium, and lumen estimated by using hybrid multidimensional MRI and corresponding T2, ADC, and histologic maps with cancer sites (Gleason score 3+3) marked. Composite map displays three tissue components in one image by using volume fractions of stroma (green), epithelium (red), and lumen (blue). Cancers appear red due to increased epithelium and loss of lumen and stromal volume. Cancer was predicted based on a fractional volume of epithelium higher than 40% and fractional volume of lumen less than 20%. Images courtesy of Radiology.
Tissue composition maps for the stroma, epithelium, and lumen estimated by using hybrid multidimensional MRI and corresponding T2, ADC, and histologic maps with cancer sites (Gleason score 3+3) marked. Composite map displays three tissue components in one image by using volume fractions of stroma (green), epithelium (red), and lumen (blue). Cancers appear red due to increased epithelium and loss of lumen and stromal volume. Cancer was predicted based on a fractional volume of epithelium higher than 40% and fractional volume of lumen less than 20%. Images courtesy of Radiology."The most important part of our tool is the fact that it is purely quantitative; therefore, it is reproducible," Oto said. "We have come up with a scale that is helpful for the detection of cancer and the differentiation of the aggressiveness of cancer, but also it is a scale that can be detected by MRI. We believe that these changes are on a scale that we can capture by using special MRI techniques."
To validate the results, the researchers are developing a follow-up prospective study that includes the University of Chicago and two other facilities. If they are successful, Oto and colleagues hope one day to use the multidimensional MRI model routinely in the clinical setting.