LAS VEGAS - Just hearing the word "audit" can make radiologists at even the most organized imaging practices start to sweat. But if an audit is done well, it can actually support -- and even promote -- a facility's radiology services, according to a presentation at the National Consortium of Breast Centers (NCBC) meeting this week.
Performing regular audits can help an imaging center survive in an era of increased pressure on healthcare systems by helping them not only cut costs, but also provide competitive quality patient care, according to Dr. Michael Linver, director of mammography at X-Ray Associates of New Mexico. Linver gave an audit primer to NCBC attendees on Monday.
There are many reasons to conduct an expanded audit, Linver said, not least of which is to meet the basic audit requirements laid out by the Mammography Quality Standards Act (MQSA). An audit can measure the performance of individual mammographers and provide data that can be used to improve performance going forward, especially through the review of false negatives. Detailed audit data can also improve patient follow-up and compliance, provide information that will help centers calculate costs, and, if necessary, provide documentation for medicolegal defense.
"The only certain and accurate assessment of clinical outcomes in mammography is the audit," Linver said. "And since mammography information has to be coded anyway with the [American College of Radiology's (ACR)] BI-RADS system, it can be fairly simple to perform an audit, especially using a computerized commercial program."
There are three major questions for screening mammography that breast imaging centers can keep in mind and evaluate with audit data:
- Are we finding a high percentage of cancers that are present?
- Are we finding a large proportion of small and node-negative cancers?
- Are we finding cancers with an acceptable number of recalls and biopsies?
"Determining your center's cancer detection rate and sensitivity, its percentage of minimal and node-negative cancers, and its overall recall rate and positive predictive value [PPV] for biopsies provides key data," Linver said.
At minimum, a breast center's audit should include the following raw data:
- Total number of mammography exams performed during a given period
- Number of screening versus diagnostic patients
- Number of recall exams
- Number of recommendations for biopsy or surgical consults
- Results of biopsies
- Tumor staging
- True-positive rate
- False-positive rate
- PPV (based on abnormal screening exams, recommendations for biopsy, and biopsy results)
- Cancer detection rate, both screening (prevalent and incident) and diagnostic
- Percent minimal cancers (ductal carcinoma in situ [DCIS] or invasive cancer 1 cm or less)
- Percent node-negative cancers
- Recall rate
Audit data can come from mammography reports (demographics, exam findings), pathology reports (biopsy findings), surgical reports (gross findings, staging), tumor registries, referring and/or consulting physicians, and patients themselves, Linver said.
With the raw data, a breast center can then gather further derived data, such as the number of cancers correctly detected by mammography per 1,000 patients examined; the minimal cancer rate (number of DCIS cases and invasive cancers less than 1 cm divided by total number of screening-detected cancers); median invasive tumor size, in centimeters; the axillary lymph node positivity rate; and sensitivity and specificity.
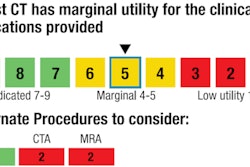
Once a center has measured its performance within its practice, it can then compare itself to the rest of the country, according to Linver. A good place to start is with the ACR's BI-RADS manual (2003), which sets out these goals for screening cases:
- PPV, abnormal screening exam: 5%-10%
- PPV, biopsy recommended: 25%-40%
- Tumors found, stage 0 or 1: 50%
- Minimal cancers found: 30%
- Node positivity: < 25%
- Cancers found per 1,000 cases: 2%-10%
- Recall rate: ≤ 10%
- Sensitivity: 85%
- Specificity: 90%
These are desirable performance goals, Linver said. And with the publication of the Breast Cancer Surveillance Consortium (BCSC) data in 2006 -- based on 1.5 million exams -- centers have real performance benchmarks for comparing their internal performance.
In fact, U.S. radiologists are doing fairly well, according to Linver:
Desirable audit goals versus diagnostic benchmarks
|
||||||||||||||||||||||||||||||||||||||||
| *Agency for Health Care Policy and Research Data courtesy of Dr. Michael Linver. |
||||||||||||||||||||||||||||||||||||||||
But there are limitations to comparing individual audit data to desirable goals and published benchmarks, Linver said.
"In individual center audits, there are much smaller numbers, differences in patient populations, and differences in the extent of follow-up [when compared to national data]," he said.
In any case, audit data can be used to improve a center's outcomes: Each radiologist's performance can be compared to the others in the same group, and that performance can be followed over time. If the performance of a particular radiologist is poor, the center can offer the individual remedial training, Linver said.
And, of course, audit data can improve group outcomes as well. Breast imaging centers should review data as a group, paying special attention to sensitivity and PPV performance, as well as evaluating true positives (cancer detection rate, tumor size, node positivity) and false negatives.
"Assessing the cause of false negatives -- was it the technologist or the interpretation? -- is crucial," Linver said. "Then take corrective action."
There are some roadblocks to a successful audit, including the complexity of the center's system in its reporting and coding of data, patient migration and use of other providers, referral patterns, biopsies conducted at other institutions, absence of a tumor registry, and audit costs, both direct and indirect. But it's still worthwhile to try, according to Linver, especially because changes in the MQSA audit requirements may be coming soon, and the national trend toward "value-based purchasing" is here to stay. But the real benefit of medical auditing goes to patients.
"The moral of the story? Do a complete audit anyway," Linver said. "The real winners are the women we see every day in our practices."