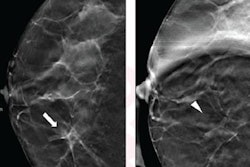
Ultrasound should be the first line for diagnostic workup of noncalcified masses recalled from digital breast tomosynthesis (DBT) exams, according to research published December 15 in the American Journal of Roentgenology.
A team led by Dr. Jessica Porembka from the University of Texas Southwestern Medical Center found that ultrasound by itself is effective in diagnostically evaluating noncalcified masses recalled on screening DBT.
However, for asymmetries, the researchers also found that diagnostic mammography may be best without additional ultrasound, while architectural distortions still warrant mammography and ultrasound.
"Ultrasound should be considered the first-line diagnostic workup of masses recalled from screening DBT," Porembka and colleagues said. "Asymmetries may be resolved with diagnostic mammography alone without the need for additional ultrasound, whereas architectural distortions benefit from continuing the traditional practice of diagnostic mammography followed by ultrasound."
DBT has seen increased use in the U.S. over the past 10 years following clearance of the first systems. The study authors said this is due to the technology's increased cancer detection rate and lower recall rate compared with conventional digital mammography.
This is leading to a repositioning of diagnostic mammography for evaluating suspicious abnormalities found on screening. Porembka et al said that many radiologists evaluate recalled findings from screening DBT with additional mammographic views prior to ultrasound or biopsy.
"The increasing use of screening DBT presents opportunities to modify the practice of performing diagnostic mammography for the evaluation of recalled lesions," the authors wrote.
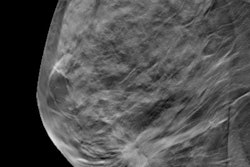
The researchers said that diagnostic mammography compression views may still be needed because asymmetries and focal asymmetries can represent undercompressed breast tissue. In the current study, they wanted to compare the performance of diagnostic evaluation using breast ultrasound alone versus ultrasound and additional mammographic views for noncalcified findings recalled from screening mammography with DBT.
"The hope was that our study may provide much-needed evidence to help change clinical practices to reduce unnecessary diagnostic mammograms, while also improving patient experiences, optimizing workflows, and decreasing radiation and cost," Porembka told AuntMinnie.com.
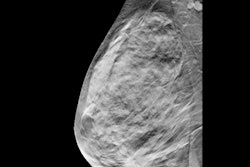
The team looked at data collected between 2017 and 2019 from 430 recalled noncalcified lesions in 399 women with an average age of 60. Ultrasound alone was performed on 306 of the total lesions, while ultrasound with diagnostic mammography was performed on the other 124 lesions.
Recalled abnormalities with a BI-RADS 1 assessment were significantly more likely to have been evaluated with ultrasound and mammography than with ultrasound alone (p < 0.001). However, masses were significantly more likely than other recalled findings to be resolved with ultrasound alone.
Ultrasound alone "adequately" evaluated 93.7% of recalled masses (178/190). Of the 93 lesions that underwent needle biopsy, 38 were found to be invasive cancers. Ultrasound alone evaluated 35 of these cancers, while the remaining three were evaluated with ultrasound and diagnostic mammography. Ultrasound alone had a sensitivity of 94.9% for cancer diagnosis.
At median follow-up of 25 months, six cancers were identified in patients with initially benign workup. Three of these were with ultrasound alone while the other three were with ultrasound plus diagnostic mammography. Ultrasound alone had two false-negative cancers.
"Omitting diagnostic mammography when ultrasound is negative has a low false-negative rate," the study authors wrote.
Porembka told AuntMinnie.com that the team is looking at "many" different areas of this study for future research, including cost analyses.