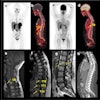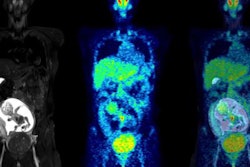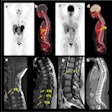
Should PET/CT be used in pregnant women with suspected cancer? Experts recommend against it, but a recent survey of nuclear medicine physicians in Australia indicates a majority would consider it in carefully selected cases, according to an article published October 18 in the Internal Medical Journal.
Researchers at the University of New South Wales in Sydney conducted a survey of nuclear medicine physicians to assess practice and attitudes with respect to PET/CT in pregnancy. They found 27% had direct experience, while 98% responded with a "yes" or "maybe" when asked if they would consider performing diagnostic PET/CT in pregnant women.
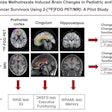
"There is emerging evidence that likely absorbed fetal doses in pregnancy are relatively low, and as such in certain circumstances PET/CT may be acceptable when balancing benefit and risk," wrote lead author Dr. Pietro Di Ciaccio of St. Vincent's Hospital in Sydney and colleagues.
Most guidelines and expert opinions recommend against the use of PET/CT in pregnancy, due to unknown fetal safety concerns. However, some studies suggest PET/CT should not be absolutely contraindicated in pregnancy, with a growing body of evidence that minor fetal absorbed doses in PET/CT may be acceptable when balanced against the therapeutic benefit to the mother, according to the authors.
To gain insight on physicians' perspectives on the issue, the researchers designed a nine-item email survey regarding the practice and experience of nuclear medicine physicians in Australia.
A total of 33 nuclear medicine physicians participated in the survey between May 2020 and July 2020. The level of professional experience of respondents was high, with the majority (69%) of respondents practicing for more than 15 years, and 47% for more than 20 years. The completion rate of the survey was 94%.
The study authors found that 27% (9/33) of respondents had direct experience performing PET/CT in pregnant women. Of those, 15% (5/33) had experience specifically with pregnant women with lymphoma.
If respondents indicated that they did not have experience with PET/CT, they were asked if they would consider performing studies in carefully selected patients with appropriate multidisciplinary consultation. Out of the 25 responses to this question, 56% of respondents indicated "yes" and a further "36%" indicated "maybe."
Finally, respondents were asked which of the following modifications they would consider important for PET/CT in pregnant women:
- Reduced radiopharmaceutical dose
- Reduced milliampere seconds (mAs) or kilovoltage peak (kVp) of the CT component of the study, if performed
- Formal dosimetric calculations
- Intravenous fluids, forced diuresis
- The placement of an indwelling urinary catheter
Among responses, reduction in radiotracer dose was the most consistent modification considered important (30/31). Reduced mAs or kVp of the CT was also nominated by 87% as important (27/31).
Although expert guidelines tend to discourage the utilization of PET/CT in pregnancy, this position is based on uncertainty, rather than on firm evidence, the authors wrote. It is important to continue to define the role of PET/CT in pregnancy, particularly as this imaging modality has emerged as the standard of care in staging and response assessment for many cancers, they added.
"Ultimately, the guiding principle ought to be a judicious balance between likely therapeutic benefit of PET/CT versus potential maternal and fetal harm from radiation exposure," the team concluded.