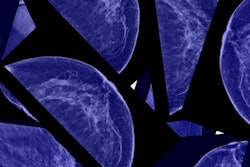
Screening with digital breast tomosynthesis (DBT) boosts specificity compared with 2D mammography and also finds more cancers, particularly those associated with better prognoses, according to a study published online February 28 in JAMA Oncology.
The study showed that these benefits are seen in women of all ages and breast tissue types, lead author Dr. Emily Conant of the University of Pennsylvania in Philadelphia told AuntMinnie.com via email.
"Controversy over breast cancer screening guidelines continues to center around the risk-benefit balance -- minimizing false positives while maintaining or even increasing the detection of clinically significant cancers," Conant said. "Our findings again support that DBT screening provides these improvements across all ages and breast densities."
Better outcomes
 Dr. Emily Conant from the University of Pennsylvania.
Dr. Emily Conant from the University of Pennsylvania.DBT screening has already been associated with fewer false positives and increased breast cancer detection rates. But what cancers does the technology find, and are they different than those identified by 2D mammography?
To address these questions, Conant's group used data from three research centers in the Population-Based Research to Optimize the Screening Process (PROSPR) consortium. The data included 96,269 women who underwent 180,340 breast cancer screening exams between January 2011 and September 2014. Of these exams, 71.7% were performed with 2D digital mammography, and 28.3% were performed with DBT. The group tracked the following performance measures: biopsy rate, cancer detection rate per 1,000 exams, sensitivity, specificity, positive predictive value of positive screening result (PPV1), and positive predictive value of biopsies performed (PPV3).
The researchers found that both modalities had higher recall rates for younger women, women with dense breasts, and those having their first screening exam. But the DBT rate was lower than the 2D mammography rate across all age groups and densities, particularly among younger women at 16.3% for 2D mammography and 11.7% for DBT, the team noted.
DBT had higher breast cancer detection rates across all age groups and densities, although this was especially apparent among younger women with nondense tissue (1.7 per 1,000 women higher than with 2D mammography) and women of all ages with dense breasts (2.27 per 1,000 women higher than with 2D mammography).
| Outcomes comparison: 2D mammography and DBT | ||
| Performance measure | Digital mammography | DBT |
| Biopsy rate per 1,000 exams | 19 | 28 |
| Cancer detection rate per 1,000 exams | 4.8 | 6.4 |
| Sensitivity | 91.5% | 90.6% |
| Specificity | 88.9% | 91.3% |
| PPV1 (positive screening result) | 3.9% | 6.3% |
| PPV3 (biopsies performed) | 24.6% | 22.3% |
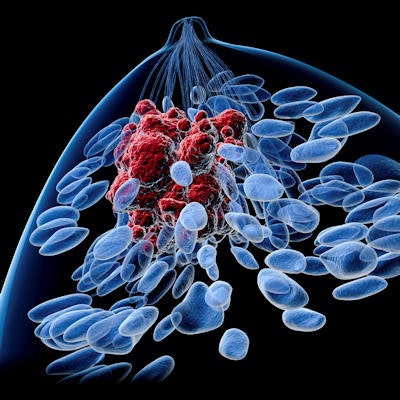
The researchers also found that DBT screening identified invasive cancers that were more often smaller, node-negative, and human epidermal growth factor receptor 2 (HER2)-negative, compared with 2D mammography.
"This was especially true for women ages 40 to 49, where the largest shift toward better prognosis cancers was found -- only 25% poor prognosis with DBT in this age group versus 40.4% with 2D mammography," Conant told AuntMinnie.com. "Therefore, we believe that DBT screening has a very favorable risk-benefit ratio, especially in the very controversial group of younger women."
The research builds on what has already been demonstrated regarding DBT's strengths compared with 2D mammography, and it highlights DBT's ability to identify cancers that have characteristics associated with better outcomes for women, according to Conant.
"DBT should be the standard of care," she said.