Three-dimensional volumetric MR images of cervical disease yield a bounty of critical information, enabling precise planning of brachytherapy for residual tumors, according to researchers from St. Joseph's Hospital and Medical Center in Phoenix.
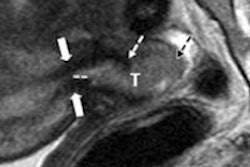
These 3D volumetric images, reconstructed from an isotropic 3D T2-weighted fast spin-echo (FSE) sequence, facilitate excellent multiplanar tumor visualization, quantitative tumor burden assessment, and precise individual temporal response analysis for planning brachytherapy, according to the team led by Dr. Olga Kalinkin, PhD.
"This 3D technique allows us to visualize anatomical borders of the tumor as a volume," Kalinkin, an associate professor of radiology at Creighton University School of Medicine and St. Joseph's Hospital and Medical Center, told AuntMinnie.com.
Kalinkin described the 3D method during a presentation at the recent American Roentgen Ray Society (ARRS) annual meeting in Washington, DC.
Working as a team
Cervical cancer is the seventh most common malignancy worldwide. The current standard of care for carcinoma of the cervix stages IIb to IV is radiation therapy with chemotherapy. While the use of intracavitary brachytherapy is essential in curative therapy, its success requires the delivery of a high radiation dose directly to the tumor while sparing the surrounding normal tissue, Kalinkin said.
She emphasized that fighting cancer is a team effort at her institution.
"We have the gynecological oncology team of specialists, including the gynecological surgeons, the radiation oncologist, the gynecological pathologist, the genetic consult, and the radiologist, working together to diagnose, stage, and treat the gynecological cancers with the most advanced technology and treatment regimes," Kalinkin said. "We enroll our patients into the different trials with application of new medications, including some medications from the [Translational Genomics Research Institute]."
The radiation oncologist needs to see the tumor margin in three dimensions to provide accurate delivery of radiotherapy to the cervical cancer, she said. Ideally, dose should be prescribed to the individual patient's tumor volume.
Not only can the 3D T2-weighted MRI sequence visualize the tumor margins at 1- to 2-mm resolution, it can also -- following reconstruction -- enable precise calculation of tumor volume, according to Kalinkin.
"This is advantageous compared to the traditional tumor diameter response assessment by [Response Evaluation Criteria in Solid Tumors (RECIST)]," she said.
Different targets
Cervical cancer is heterogeneous; not all cervical tumors are the same. Some tumors are very sensitive to radiation and demonstrate a dramatic response, with a significant decrease in tumor burden volume seen during MRI follow-up. However, other more resistant cervical neoplasia require modifications of the radiation dose within the tumor burden, Kalinkin said.
 3D model of uterine corpus (white color) and cervical cancer (red color) after reconstruction of a 3D T2-weighted sequence.
3D model of uterine corpus (white color) and cervical cancer (red color) after reconstruction of a 3D T2-weighted sequence. Calculated volume of cervical tumor. All images courtesy of Dr. Olga Kalinkin, PhD.
Calculated volume of cervical tumor. All images courtesy of Dr. Olga Kalinkin, PhD."This 3D technique allows us to visualize anatomical borders of the tumor as a volume," she said.
A single-slab 3D FSE T2-weighted imaging sequence can acquire near-isotropic 3D volume data within an acceptable scan time, and it allows for high-resolution, thin 2-mm reformatted images in any arbitrary plane (i.e., true axial, sagittal and coronal, or any oblique orientation), Kalinkin said. This yields clinical advantages for evaluating complex anatomical detail, pathology, and small lesions.
The researchers studied the utility of the 3D FSE sequence and associated postprocessing methods on 15 patients (age, 31-52 years) with histologically confirmed stage IIb-IV cervical cancer. All patients were prospectively imaged with interval MRI over 26 to 63 days. The first study was performed prior to commencing external-beam therapy, while the second MRI was obtained to delineate residual cervical tumor for brachytherapy planning, according to the researchers.
MRI was performed on a Signa LX 1.5-tesla scanner (GE Healthcare) using an 8-channel body phased-array coil, vaginal gel, and a three-plane localizer. The isotropic sagittal 3D FSE T2 sequence (TR/TE, 2,000/90; matrix, 256 × 256; field-of-view, 26 cm; section thickness, 2 mm) was acquired as part of the site's dedicated female MRI protocol. Multiplanar reformatting was performed in the axial, coronal, and paraxial planes.
The cervical tumor was measured in three dimensions. In addition, each patient was evaluated for parametrial tumor extension, uterine corpus extension, vaginal extension, pelvic lymph node involvement, and direct tumor extension.
Postprocessing
Postprocessing was performed on an Advantage Windows 4.4 workstation (GE) with a 3D volume-rendering program. After 3D tumor segmentation was complete, the researchers calculated 3D tumor volume. 3D color coding was then performed and a cervical mass model was produced.
Kalinkin and colleagues found that the initial absolute volume of local cervical disease ranged from 28 cm3 to 185 cm3. Individual patient response to external-beam radiation therapy also varied; residual tumor volume ranged from 2 cm3 to 51 cm3, with complete resolution in one patient.
The radiation oncologist used the 3D color-coded image to precisely plan brachytherapy for the residual cervical tumor.
The group concluded that the 3D T2 FSE sequence offered great visualization of cervical cancer for regional staging. It also supports multiplanar reconstruction in any needed plane, she said.
"After this sequence was processed with volume rendering software, the additional clinical information retrieved, such as absolute tumor volume and 3D spatial tumor distribution, [facilitated] initiation and increasing precision of targeted brachytherapy," Kalinkin said.
Limitations
Kalinkin acknowledged several limitations of the study, including its small group of patients and its single-reader format. In addition, a few cervical cancers are minimally T2-hypertense with limited visualization by a 3D FSE T2 sequence alone. Furthermore, a 3D FSE T2 sequence could be degraded by motion in difficult clinical situations, she said.
Nonetheless, the application of a near-isotropic 3D sequence in cervical cancer was shown to enable tumor visualization and traditional regional tumor staging, Kalinkin said.
"This sequence provides calculation of absolute tumor burden and spatial volume distribution," she concluded. "Retrieved from this sequence, a 3D cervical tumor model is valuable for prescription of targeted brachytherapy for relevant absolute volume of tumor."
Kalinkin also noted that the 3D MRI-reconstructed images can be fused with CT images during brachytherapy.
"The most intriguing goal is to illuminate the functional activity of cancer and predict tumor response on specific therapy," she said.