Researchers have created 3D-printed models of groin vasculature with texture resembling real tissue for use in training students on ultrasound-guided interventional procedures. They detailed their experience with the models in a March 20 talk at the Society of Interventional Radiology (SIR) 2018 annual meeting.
Stanford University researchers tested the technique in a simulation session of ultrasound-guided femoral artery access for medical students. Nearly all the students who trained for the procedure on the 3D-printed models reported that they were straightforward and beneficial, and they also increased their confidence in performing the procedure in the future.
"We've come up with a viable method for creating [a training model] that's inexpensive and also customizable to individual patients," lead author Dr. Alexander Sheu stated in a press release. "The current model used to train medical students lacks the ability to replicate a patient's anatomy. Our 3D-printed model will provide students a more realistic experience, allowing for better preparation before they perform procedures on real patients."
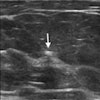
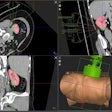
 Ultrasound-compatible, 3D-printed vascular access model. All images courtesy of Dr. Rajesh Shah, director of interventional radiology in the Veterans Affairs Palo Alto Healthcare System.
Ultrasound-compatible, 3D-printed vascular access model. All images courtesy of Dr. Rajesh Shah, director of interventional radiology in the Veterans Affairs Palo Alto Healthcare System.Inexpensive and customizable
Simulating complex procedures before performing them is becoming increasingly more common in medical training, according to the investigators. In the case of ultrasound-guided procedures, interventional radiologists typically conduct medical simulation exercises on commercial devices listed at upward of $2,000.
A relatively cost-effective alternative for purchasing a commercial device has been creating 3D-printed models, which can be customized to individual patients. Numerous surgeons and interventional radiologists have already turned to 3D printing to prepare for surgeries and practice image-guided procedures.
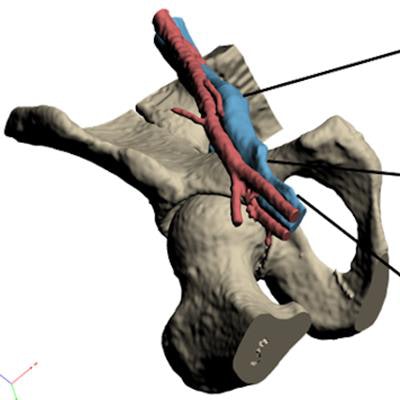
Following these precedents, Sheu and colleagues set out to assess the viability of training specifically for ultrasound-guided femoral artery access with 3D-printed vascular models. They constructed these models by segmenting and smoothing the CT scans of a patient and then sending them for production in a 3D printer.
To enhance the realism of the models, they input into the printer tissue-mimicking material that was durable enough to withstand punctures and also compatible with ultrasound scanning.
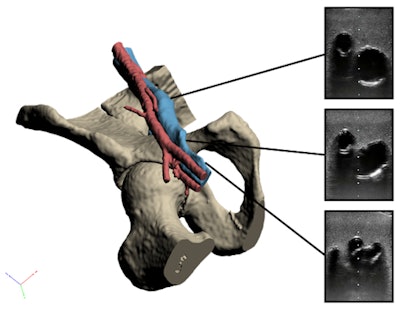 3D-reconstructed vascular model and corresponding ultrasound images of the common femoral (top), deep femoral (middle), and superficial femoral (bottom) arteries.
3D-reconstructed vascular model and corresponding ultrasound images of the common femoral (top), deep femoral (middle), and superficial femoral (bottom) arteries.Unlike commercial devices, the 3D-printed models reproduced the patient's distinct anatomy and the unique texture of the patient's skin, the researchers noted. Tailoring the simulation models in this way allowed the trainees to practice on variations in anatomy, which could ultimately help lower complication rates during actual surgery.
Among the 32 medical students who participated in the simulation, 15 trained using a 3D-printed vascular access model and 17 with a generic commercial model (FemoraLineMan, Simulab). Slightly more than 73% of the trainees in both groups said they "did not feel confident" performing femoral artery access prior to the simulation, and only one student had ever attempted the procedure beforehand.
Improving procedural skills
After completing the training, nearly all the students claimed that both the 3D-printed model and the commercial device were "easy to use" and "helpful."
| Procedural training with commercial device vs. 3D-printed vascular access model | ||
| Students' experience | Commercial device | 3D-printed vascular model |
| Easy to use | 94.1% | 93.3% |
| Helpful for training | 94.1% | 93.3% |
In addition, the researchers found a statistically significant increase in subjective student confidence for both groups after training (p ≤ 0.001).
"Now that we know that a 3D-printed model is just as effective at training medical students in this type of procedure, this simulation experience can be made available to even more trainees and potentially improve procedural skills for residents, fellows, and attendees," Sheu noted. "We foresee this really making an impact in the world of interventional radiology training."
Their experience has encouraged the researchers to start developing similar 3D-printed vascular models of other areas of the body and offer their training scheme to residents and fellows as well.