The additional information provided by preoperative prostate MRI influenced the extent of surgery in 27% of patients who underwent robotic-assisted laparoscopic prostatectomy (RALP), according to a new study published online January 24 in Radiology.
Initial surgical plans were changed in 28 of 104 patients, with 17 cases changed to a nerve-sparing technique and 11 altered to a non-nerve-sparing technique. In patients whose surgical plan was changed to the nerve-sparing technique, researchers found no positive margins on the side of the prostate after the change in treatment plan.
Study co-author Dr. Daniel Margolis said preoperative MRI is useful for surgeons who are uncertain whether to spare or resect the nerves. Compared with clinical information alone, MRI is worthwhile for all patients because the modality identifies important information leading to a change in the surgical plan in almost a third of patients. The lead author of the study was Dr. Timothy McClure, from the department of radiology at the University of California, Los Angeles's (UCLA) David Geffen School of Medicine (Radiology, March 2012, Vol. 262:3; online January 24).
RALP benefits
Robotic-assisted laparoscopic prostatectomy is considered to be better for patients because the technique uses smaller incisions than open radical prostatectomy and offers better cosmetic results with less blood loss and a shorter postoperative recovery.
However, as the authors noted, surgeons performing RALP lack tactile feedback, which can compromise their ability to evaluate blood vessels and nerves adjacent to the prostate. If a surgical approach is too aggressive, neurovascular bundles could be damaged, resulting in a loss of function for patients. On the other hand, a less aggressive approach may not remove all the cancer from a patient's prostate.
The UCLA researchers prospectively evaluated 104 consecutive men between January 2004 and April 2008 with biopsy-proven prostate cancer. All subjects underwent preoperative T2-weighted endorectal coil 1.5-tesla MRI (Magnetom Avanto, Siemens Healthcare) and follow-up RALP.
Of the 104 patients, 88 received diffusion-weighted imaging (DWI-MRI), 51 had dynamic contrast-enhanced MRI, and 91 underwent spectroscopy.
The researchers evaluated any differences in surgical plans from before and after MRI, and they compared the plans to the surgical and pathologic results.
Surgical strategies
Preoperative prostate MRI data changed the decision to use a nerve-sparing technique during RALP in 28 (27%) of 104 patients, according to the group. Surgeons changed to the nerve-sparing technique in 17 (61%) of the 28 patients and to a non-nerve-sparing technique in 11 patients (39%). The decision to opt for nerve-sparing surgery did not compromise oncologic outcome.
The researchers found no positive margins on the side of the prostate where there was a change in treatment plan. "Some patients thought to require non-nerve-sparing surgery might safely undergo nerve-sparing surgery on the basis of MR imaging findings because this change in surgical plan does not appear to be associated with an increase in positive surgical margins," the authors wrote.
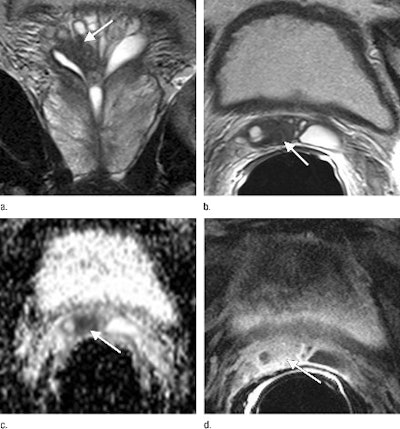 |
| The surgical plan for this 53-year-old man was changed to a non-nerve-sparing technique after review of coronal (a) and axial (b) T2-weighted images that show a low-signal-intensity mass (arrow) extending into the right seminal vesicle. Apparent diffusion coefficient map (c) shows restricted diffusion (arrow), corresponding to the low-signal-intensity focus on T2-weighted images. Contrast-enhanced fat-saturated T1-weighted gradient-echo image (d) shows enhancing nodule (arrow), corresponding to the area of low signal intensity on T2-weighted images. Images courtesy of Radiology. |
Of 173 sides in which nerve-sparing surgery was initially planned, 168 (97%) were stage T2 cancer, according to MRI results. The specificity of prostate MRI in differentiating T2 disease from T3 disease was 98%.
"This suggests that, in our patient population, if a patient's prostate MR image shows T2 disease, a nerve-sparing technique can be used with a high degree of safety and without compromising oncologic outcome," the authors wrote.
The researchers emphasized that the 104 patients represented a population of men with low- to medium-grade cancer, and that the findings might not apply to all patients.
For preoperative MRI to become more commonplace, there must be a better way to determine which patients would benefit from the technique, and a more standardized means of acquiring and interpreting prostate MRI results, McClure and colleagues noted. Which patients would be helped most by preoperative prostate MRI is the focus of their follow-up research.