Brain MRI scans have shown that COVID-19 can include neurologic manifestations such as acute stroke and altered mental status, according to a research letter published May 8 in Radiology.
In fact, almost half (44%) of patients in the intensive care unit with COVID-19 and neurologic symptoms had abnormal MRI findings, wrote a team led by Dr. Sedat Kandemirli of the University of Iowa Hospital and Clinics in Iowa City. Additionally, the rate of neurological symptoms was higher in those patients with more severe respiratory disease.
"The relatively high percentage of neurologic symptoms is concordant with studies showing neurotropism of coronavirus," the group wrote.
Currently scarce data is available regarding neuroimaging findings in patients with COVID-19, such as acute hemorrhagic necrotizing encephalopathy and meningoencephalitis, the authors noted. So Kandemirli and colleagues sought to describe findings on brain MRI in intensive care patients with the disease.
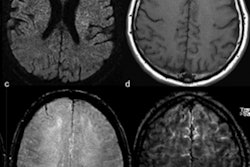
The study included 50 of 235 patients with COVID-19 admitted to the intensive care unit (ICU) between March 1 and April 18 who developed neurological symptoms. Of these 50 individuals, 27 underwent brain MRI scans (54%); 44% had acute findings. Ten of the 27 patients who had brain MRI showed cortical signal abnormality on fluid-attenuated inversion-recovery (FLAIR) protocols; three patients showed accompanying subcortical and deep white-matter signal abnormality on FLAIR images.
The researchers also found the following brain MRI results:
- Four patients had frontal lobe abnormalities, while three had abnormalities in the parietal lobe, four in the occipital lobe, one in the temporal lobe, three in the insular cortex, and three in the cingulate gyrus.
- Of 10 patients with cortical signal abnormalities, cerebrospinal fluid was sampled from five. Four of these patients had elevated total protein (mean 79.9 mg/dL).
- One patient had acute transverse sinus thrombosis and one patient had acute infarction in the right middle cerebral artery area -- both of whom did not have accompanying cortical signal abnormality.
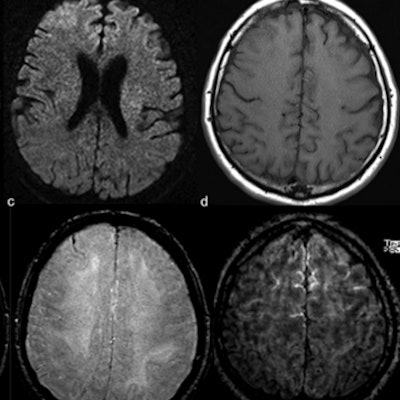
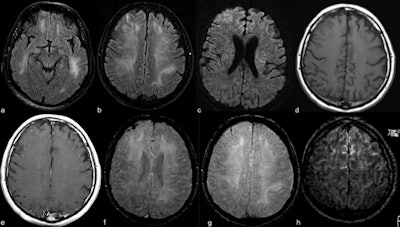 Contrast-enhanced cranial 1.5-tesla MRI examination of a 59-year-old intubated male patient with altered mental status despite tapering of sedoanalgesia. Axial FLAIR images at level of midbrain (a) and centrum semiovale (b) demonstrate prominent symmetric white matter hyperintensity and right frontal cortical hyperintensity. There is also prominent linear hyperintensity within frontal sulci. Axial b2000 DWI (c) shows frontal increased signal with corresponding low apparent diffusion coefficient (ADC) (images not provided). Axial T1-weighted imaging (T1WI) (d) shows right frontal sulcal effacement. Postcontrast T1WI (e) shows mild pial-subarachnoid enhancement. Axial susceptibility-weighted imaging (SWI) at the level of corona radiata (f) and centrum semiovale (g) demonstrates blooming artifact in the frontal sulci. Postcontrast FLAIR (h) depicts the bilateral leptomeningeal enhancement. Caption and images courtesy of the RSNA.
Contrast-enhanced cranial 1.5-tesla MRI examination of a 59-year-old intubated male patient with altered mental status despite tapering of sedoanalgesia. Axial FLAIR images at level of midbrain (a) and centrum semiovale (b) demonstrate prominent symmetric white matter hyperintensity and right frontal cortical hyperintensity. There is also prominent linear hyperintensity within frontal sulci. Axial b2000 DWI (c) shows frontal increased signal with corresponding low apparent diffusion coefficient (ADC) (images not provided). Axial T1-weighted imaging (T1WI) (d) shows right frontal sulcal effacement. Postcontrast T1WI (e) shows mild pial-subarachnoid enhancement. Axial susceptibility-weighted imaging (SWI) at the level of corona radiata (f) and centrum semiovale (g) demonstrates blooming artifact in the frontal sulci. Postcontrast FLAIR (h) depicts the bilateral leptomeningeal enhancement. Caption and images courtesy of the RSNA."Current evidence suggests an association of neurologic manifestations with COVID-19 infection including acute stroke and altered mental status," the group wrote. "Neurotropism of coronavirus may account for the relatively high percentage of neurologic involvement. In addition to neurotropism, another potential mechanism for neurologic manifestations might be related to cytokine storm syndrome."
Kandemirli and colleagues hope the research will help those on the front lines of the COVID-19 pandemic to best care for patients.
"[Our] report may help increase awareness for possible neurological involvement of SARS-CoV-2 for patients in the ICU," the team concluded.