Relief may finally be near for people who experience significant abdominal pain and discomfort. Researchers at Purdue University are developing a way to use MRI to track the efficacy of electric stimulation of the vagus nerve to alleviate stomach dysfunction, according to a paper published in the October issue of Neurogastroenterology and Motility.
Gastric issues are primarily caused by the stomach's inability to properly empty digested food into the small intestine. Stimulation of the vagus nerve, which helps control stomach muscle movement, is seen as a possible solution. MRI's role would be to verify the most effective level of stimulation for more precise patient treatment than is currently available through drugs and dietary changes (Neurogastroenterol Motil, October 2018, Vol. 30:10).
"With the use of MRI, since it is noninvasive, we can potentially ask a patient to undergo multiple scans of MRI with different stimulation settings while we stimulate the vagus nerve," explained said Kun-Han Lu, a doctoral student in electrical and computer engineering at Purdue. "By doing so a number of times, we can potentially figure out what would be the best stimulation for this particular patient to alleviate their gastric symptoms."
Gastric disorders, such as gastroparesis and reflux disease, affect more than 60 million people in the U.S. each year and result in more than $98 billion in medical costs, according to the authors. Naturally, the stomach, which receives signals from the brain through the vagus nerve, frequently is the culprit.
"The stomach is a very coordinated organ. Some people even call the stomach a second brain," Lu said in a video describing the researchers' work. "It is very hard, at this point, for doctors to pinpoint what kind of drug or what kind of dietary treatment is best suited for [a patient's] condition."
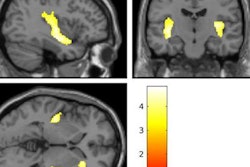
In this study, the researchers tested vagus nerve stimulation on the ability of rats to empty their stomachs after consuming a gadolinium-labeled meal after fasting. The researchers monitored how the electrical technique affected stomach muscle function and gastric emptying over time through contrast-enhanced preclinical MR images and computer-assisted 3D image processing.
The MR images showed that vagus nerve stimulation significantly accelerated gastric emptying to the point where the rats' stomachs passed along 41% of their food every four hours. The technique relaxed the pylorus (the opening from the stomach to the small intestine) and the pyloric sphincter, which, in turn, positively correlated with the enhanced gastric emptying rate.
The U.S. Food and Drug Administration (FDA) has approved some stomach stimulation protocols for humans, but the available techniques are only partially effective, added Terry Powley, PhD, a professor of neuroscience at Purdue. The ultimate goal is to validate vagus nerve stimulation and tailor it to each patient's gastric condition.
"Not every patient would have a positive outcome when they receive the same drug or the same dietary treatment, but everyone has a vagus nerve," Lu said. "Using vagus nerve stimulation, we can actually try to parametrize the stimulation setting that is optimal or is the best for each individual."