The Medical Imaging & Technology Alliance (MITA) is speaking out against changes proposed by the U.S. Centers for Medicare & Medicaid Services (CMS) to restrict payments related to new drugs to treat Alzheimer's disease.
CMS earlier this month proposed a national coverage determination (NCD) that would limit Medicare and Medicaid coverage for monoclonal antibody-based drugs like aducanumab (Aduhelm) only to people enrolled in qualifying clinical trials. The NCD would only cover one beta-amyloid PET scan per patient enrolled in a clinical trial.
But MITA said the change would restrict and delay access of Medicare beneficiaries to therapeutic treatment options, as well as exacerbate disparities based on geography, ability to travel, and race. MITA also wrote that it believes Medicare's final decision should allow both coverage of amyloid PET and make sure the right patients will have access to amyloid reduction therapies.
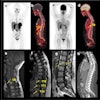
Diagnostic amyloid PET has been extensively studied since the first radiotracer was approved in 2012 by the U.S. Food and Drug Administration (FDA), MITA said. The procedure identifies amyloid plaque, one of the main characteristics of Alzheimer's disease. MITA said using amyloid PET is "clinically and fiscally responsible" by discouraging unnecessary drug use.
However, Medicare's payment methodology for PET diagnostic drugs in the hospital outpatient setting will limit provider involvement and patient access, the alliance said.
Patrick Hope, MITA executive director, said the alliance urges CMS to provide beneficiary access to Alzheimer's treatment by providing appropriate coverage and payment for amyloid reduction therapies, as well as cover and pay for FDA-approved diagnostic amyloid PET.