Adding molecular breast imaging (MBI) to conventional mammography finds more cancers in women with dense breast tissue -- and at acceptable radiation doses for screening, according to a new study published in the American Journal of Roentgenology.
The study findings are good news, as mammography's performance diminishes in dense tissue, wrote researchers from the Mayo Clinic in Rochester, MN. To address this problem, additional modalities such as ultrasound and MRI are used, but both have their own drawbacks, including ultrasound's high false-positive rates and MRI's cost. Molecular breast imaging offers another option.
"MBI produces functional images of the breast, which in my opinion is the direction we need to go to overcome the limitations of anatomical imaging in dense breast tissue," lead author Dr. Deborah Rhodes told AuntMinnie.com. "No matter how much you improve your x-ray, at the end of the day it's still an anatomical image."
Follow-up study
For this research, Rhodes and colleagues followed up a pilot study they published four years ago (Radiology, January 2011, Vol. 258:1, pp. 106-118). That initial study established that functional imaging did better than anatomical imaging in dense breasts. The current study explored how much MBI's radiation dose can be reduced while still maintaining diagnostic image quality (AJR, February 2015, Vol. 204:2, pp. 241-251).
 Dr. Deborah Rhodes from the Mayo Clinic.
Dr. Deborah Rhodes from the Mayo Clinic.The researchers included 1,585 asymptomatic women who were characterized with dense breasts based on prior mammography. The women underwent screening mammography with adjunctive MBI at a reduced dose of 8 mCi of technetium-99m (Tc-99m) sestamibi with a cadmium zinc telluride gamma camera. A conventional dose for molecular breast imaging is 20 mCi to 25 mCi. Rhodes' team used either Gamma Medica's LumaGem unit or GE Healthcare's Discovery NM 750b system for the MBI exams.
The group calculated the sensitivity, specificity, recall rates, and cancer detection rates for women with either of two categories of dense breast tissue: "heterogeneously" or "extremely" dense. Rates were calculated for mammography alone and for mammography with MBI.
Of the women included, 21 were diagnosed with breast cancer; two of these women were identified by mammography only, 14 by MBI only, three by both modalities, and two by neither modality. Of the cancers detected by MBI alone, 11 were invasive (79%), and nine of the 11 were node-negative (82%).
"Approximately 80% of cancers seen only on MBI were invasive, suggesting that MBI is not selectively detecting clinically unimportant cancers (overdiagnosis)," the authors wrote. "Eighty-two percent (9/11) of the invasive cancers seen only on MBI were node-negative, suggesting that MBI contributes to early detection of clinically important cancers."
Rhodes' group found that adding MBI to mammography increased the overall cancer detection rate per 1,000 women screened from 3.2 to 12 and the invasive cancer detection rate from 1.9 to 8.8 (the change in detection of ductal carcinoma in situ was not statistically significant). This supplemental cancer detection rate compares favorably with rates from ultrasound and tomosynthesis, the authors wrote.
| MBI + mammography vs. mammography alone | ||
| Mammography alone | Mammography + MBI | |
| Sensitivity | 24% | 91% |
| Specificity | 89% | 83% |
| Recall rate | 11% | 17.6% |
| Biopsy rate | 1.3% | 4.2% |
| Hetergeneously dense tissue | 4 cancers | 13 cancers |
| Extremely dense tissue | 1 cancer | 3 cancers |
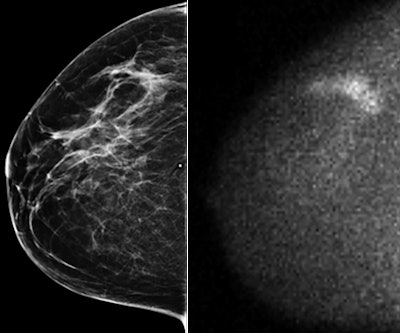 Mammographically occult invasive lobular carcinoma detected by MBI in a 54-year-old woman. Right craniocaudal image (at left) from digital screening mammography was interpreted as negative. Adjunct craniocaudal MBI image (at right) was interpreted as multifocal area of marked radiotracer uptake in upper outer right breast. Final pathology was multifocal node-negative grade I invasive lobular carcinoma more than 4 cm in extent on MBI, with largest individual mass being 0.6 cm. Images reprinted with permission from AJR.
Mammographically occult invasive lobular carcinoma detected by MBI in a 54-year-old woman. Right craniocaudal image (at left) from digital screening mammography was interpreted as negative. Adjunct craniocaudal MBI image (at right) was interpreted as multifocal area of marked radiotracer uptake in upper outer right breast. Final pathology was multifocal node-negative grade I invasive lobular carcinoma more than 4 cm in extent on MBI, with largest individual mass being 0.6 cm. Images reprinted with permission from AJR.What do the increased recall and biopsy rates tell us? Again, it's about context, Rhodes said.
"When any modality is added to mammography, the recall and biopsy rates go up -- with the exception of tomosynthesis," she said. "But our recall rate of 17.6% needs to be put in context with recall rates above 25% for supplemental automated breast ultrasound and handheld ultrasound in dense breasts. It's important for women to ask themselves what the primary reason is for pursuing supplemental imaging. It's not necessarily to lower the recall rate, but to increase cancer detection."
Radiation dose
How much additional radiation dose did the women receive? The dose of Tc-99m sestamibi used in the study corresponds to an effective whole-body dose of 2.4 mSv, according to the researchers. However, when accounting for known sestamibi adherence to the syringe, the administered activity was closer to 2 mSv, Rhodes told AuntMinnie.com.
Although the dose is higher than the average effective dose from digital mammography (approximately 0.5 mSv) and the effective dose of digital mammography combined with tomosynthesis (1.2 mSv), it is still below natural background radiation levels (U.S. annual average of 3 mSv).
"There certainly are circumstances under which patients receive too much radiation," Rhodes said. "But concern about a radiation level in the range of 2 mSv is not biologically warranted. The key is to put it in context for patients. If we tell them adding MBI to mammography doubles the dose of a mammography exam, of course that doesn't sound good. But if the goal is to find cancer in the dense breast, then having a test with a high likelihood of detecting cancer is important, even if that means a higher but still safe amount of radiation."



















