Reporting of breast tissue density needs to be standardized in the U.S. so that women are apprised of their density category even if they don't have dense tissue, according to a March 24 study in the Journal of the American College of Radiology.
Whether women receive notice of their tissue density regardless of category varies by state, and this could be causing unnecessary confusion, wrote a team led by Rebecca Smith of Dartmouth College in Lebanon, NH.
"Notification requirements vary substantially by state with some mandating reporting of breast density for all mammography encounters and others only if the woman had dense (heterogeneously or extremely dense) breasts," the group explained. "Variable reporting of breast density information may confuse women and limit the impact of state-based legislation."
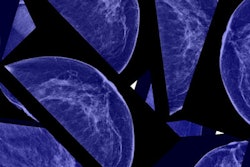
Dense breast tissue is a risk factor for breast cancer due to the masking effect it can have on mammography. Over the last decade, efforts have been made to establish notification practices to make women aware of their own tissue density on mammography screening, and, if appropriate, to encourage additional screening.
In 2019, the U.S. Food and Drug Administration proposed updates to the Mammography Quality Standards Act that would require facilities to report breast density information no matter what the category to women and their providers; this proposal remains pending, the group noted. Currently, 38 states and Washington, DC, have put density notification laws in place (this count from density education organization DenseBreast-info.org).
Smith's group investigated women's understanding of the risks of having dense breast tissue and how various notification protocols may affect this understanding. The team conducted a survey study that included 1,528 women between the ages of 40 and 74 with no prior breast cancer; a normal screening mammogram in the previous year; and one or fewer recorded breast density measures in four Breast Cancer Surveillance Consortium (BCSC) registries with density reporting requirements.
The researchers compared agreement between the women's self-reported breast density and their BI-RADS score within the previous five years and assessed women's knowledge of the implications of having dense breast tissue and their feelings about breast cancer screening.
Of survey participants, more than half (59%) had dense breast tissue. The investigators found that agreement between the women's self-reporting regarding their breast tissue density and clinically measured density was 76% among those with dense tissue and 14% among those without.
Women with dense tissue had more interest in supplemental screening compared to women who reported having nondense tissue (29% compared to 15%). But women with nondense tissue in states that report density regardless of category were 6.3 times more likely to have accurate understanding of the ramifications of having dense breasts.
Surprisingly, 62% of the women surveyed knew that dense breast tissue makes it more difficult to find breast cancer, but only 13% knew that having dense tissue translates to increased breast cancer risk.
Implementing breast density notification regardless of category in all states may boost awareness among both women and their doctors about how density affects mammography and whether supplemental imaging is in order, according to the authors. But notification alone won't do the job: Doctors need support for helping patients with dense tissue decide whether to undergo additional screening.
"Our results emphasize a need for both improved density communication and tools to support supplemental screening discussions; this need is heightened by pending implementation of national density-reporting regulations," Smith's group concluded.