An analysis of more than 300,000 Medicare patients being evaluated for heart disease found that those who received coronary CT angiography (CCTA) were more likely to go on to invasive cardiac procedures such as catheterization compared with those who received myocardial perfusion scintigraphy (MPS), according to results published in the November 16 Journal of the American Medical Association.
Compared with MPS, CCTA more than doubled the odds of subsequent cardiac catheterization, percutaneous coronary intervention (PCI), or coronary artery bypass graft (CABG) surgery, wrote Dr. Jacqueline Baras Shreibati; Laurence Baker, PhD; and Dr. Mark Hlatky from Stanford University.
"This study documents that patients who undergo CCTA frequently undergo additional cardiac testing, particularly cardiac catheterization, and subsequent coronary revascularization with PCI or CABG surgery," the authors wrote.
The results contrast to those of a couple of earlier reports, inviting speculation about what drove the differences. For example, Dr. James Min and colleagues found that patients without coronary artery disease who received CCTA had 16% lower follow-up costs than patients who received MPS, with no differences in the rates of myocardial infarction.
The study data are interesting, but follow-up in thousands of mostly younger patients since the original study was published confirms the low rate of revascularization in patients undergoing CCTA, Min, from Cedars-Sinai Medical Center, told AuntMinnie.com.
Another cardiac imaging researcher said the problem with MPS is that it misses disease that CCTA finds, leading, perhaps inevitably, to more procedures compared to CCTA.
But significant blockages missed at MPS "are readily recognized by coronary CT angiography and will trigger revascularization," said Dr. U. Joseph Schoepf, from the Medical University of South Carolina, in an email to AuntMinnie.com.
In any case, the association of CCTA with subsequent use of cardiac tests and procedures and with clinical outcomes is not well-established, the authors noted, while acknowledging that the reasons are unclear.
"CCTA might reduce follow-up testing and thus reduce expenditures by excluding significant [coronary artery disease (CAD)], as has been demonstrated among low-risk patients evaluated in the emergency department for acute chest pain," they wrote. "On the other hand, CCTA may detect atherosclerotic plaques that are not hemodynamically significant and lead to additional tests and procedures, such as coronary catheterization and revascularization, that would not otherwise have been performed, thereby increasing expenditures," (JAMA, November 16, 2011, Vol. 306:19, pp. 2128-2136).
Utilization and spending
The study aimed to compare utilization and spending associated with both anatomic testing CCTA and functional testing with MPS.
The observational cohort study was based on Medicare claims data from a 20% random sample of Medicare fee-for-service beneficiaries from 2005 to 2008. All patients were 66 years or older, had no claims related to coronary artery disease in the preceding year, and received nonemergent outpatient testing for coronary artery disease. The 282,830 patients in the 20% sample had a mean age of 73.6 years, 46% were men, and 89% were white.
CPT codes were used to identify patients undergoing CCTA, stress echo, exercise electrocardiography (ECG) tests, or pharmacological stress testing. For MPS, patients had to have undergone both a stress test and an associated imaging test within a one-day window.
The study tracked CAD-related procedures, hospitalizations, and spending for 180 days following the index test; sensitivity analysis was conducted at 90 days. Calculations of costs related to coronary artery disease testing and care included actual Medicare expenditures, including inpatient and outpatient services. All models were controlled for confounding factors including age, sex, weight, tobacco use, and comorbidities.
Among the 282,830 who underwent noninvasive testing for suspected coronary heart disease, MPS was the most common diagnostic test, used in 46.8% of cases (n = 132,343), followed by stress echocardiography at 28.5% (n = 80,604), exercise ECG at 21.6% (n = 61,063), and CCTA in 3.1% of cases (n = 8,820).
Patients undergoing CCTA were somewhat younger (mean age, 73.56 years) and had fewer comorbid conditions, including Framingham risk factors (diabetes, tobacco abuse, hyperlipidemia, hypertension), than patients undergoing MPS (mean age, 75.71 years). However, they were somewhat older and had more comorbid conditions than patients undergoing stress echocardiography (mean age, 73.80 years) or exercise ECG (mean age, 73.15 years).
Significant findings included the following:
- Compared to patients who underwent MPS, those who underwent CCTA were nearly twice as likely to undergo subsequent cardiac catheterization (22.9% versus 12.1% for MPS).
- CCTA patients were more than twice as likely to undergo coronary artery bypass graft surgery (3.71%) compared to MPS patients (1.29%).
- CCTA patients remained a little healthier over time, with a slightly lower likelihood of hospitalization for acute heart attack (0.19%) in the first 180 days after their first test than patients undergoing MPS (0.43%). But patients undergoing CCTA had a similar likelihood of all-cause mortality (1.05%) compared to patients whose testing began with MPS (1.28%).
- As for costs, both average total spending ($29,719) and spending related to coronary artery disease ($14,943) over the 180-day follow-up period were significantly higher among patients undergoing CCTA, who had nearly 50% higher CAD-related average expenditures than patients undergoing MPS.
- However, CCTA patients had lower associated spending with echocardiography (-$4,981) and exercise ECG (-$7,449) versus MPS patients.
- Overall spending related to coronary artery disease was $11,437 for CCTA versus $7,430 for MPS. Average total spending was also significantly lower for patients undergoing MPS ($29,719 for CCTA versus $14,943 for MPS).
Shreibati and colleagues concluded that Medicare beneficiaries who underwent CCTA in a nonacute setting were more likely to undergo subsequent revascularization procedures with CABG and PCI, resulting in higher coronary artery disease-related spending than for patients who underwent stress testing.
Functional significance
One issue with CCTA is the unclear functional significance of some lesions, and as a result, current guidelines recommend initial evaluation with a noninvasive stress test in most patients, with angiography reserved for patients with positive results, they noted.
CCTA's key selling point is the potential of obtaining anatomic information about the coronary arteries noninvasively, reducing the need for subsequent cardiac testing. A negative CCTA confers a 99% likelihood of not having obstructive coronary artery disease. Still, a CCTA result "is not definitive evidence of obstructive disease," as CCTA is only 88% specific, and additional functional tests are sometimes needed, according to the authors.
The net effect of CCTA on subsequent cardiac testing is therefore uncertain, and relatively few studies have looked at the issue.
One group that did was Min et al in a 2008 study (Radiology, October 2008, Vol. 249:1, pp. 62-70). They used a large private insurance claims database to compare costs and outcomes in a cohort of younger (mean age, 57 years) patients without known coronary artery disease.
Patients undergoing CCTA had 16% lower follow-up costs than those who underwent MPS, with no difference in myocardial infarction rates or cardiac hospitalizations.
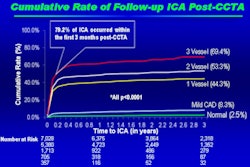
Meanwhile, a 2010 update of patients in the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes) registry found that mortality rates corresponded to significance of vessel disease at CCTA. The latest results presented in September demonstrated that patients even at low Framingham risk scores faced a high risk of adverse events if CCTA demonstrated obstructive CAD.
In a smaller study published this year, Nielsen et al found more downstream testing in the stress test group (32%) than in the CCTA group (20%) (International Journal of Cardiovascular Imaging, July 2011, Vol. 27:6, pp. 813-823).
The present JAMA study used a much larger database of 300,000 Medicare beneficiaries; however, it lacked the long-term follow-up needed to assess the long-term effects of CCTA on patient outcomes, the authors noted.
In addition, patients in private health plans may undergo fewer cardiovascular procedures than Medicare patients in general, the group said, noting that all-cause mortality was about the same for both groups of patients during the short follow-up.
Commenting on the study, Schoepf said it's important to remember that MPS and CCTA are very different tests, and that MPS is likely missing significant disease that will show up in longer-term follow-up.
The observation that CCTA is more often followed by invasive procedures and revascularization than MPS is not entirely unexpected, Schoepf wrote in his email. First and foremost, he said, the two tests do not produce identical information.
The reasons behind the higher rates are speculative, study author Hlatky told AuntMinnie.com by email. "It could be that in the older population in our study (median age of 75) it's not common to have completely normal coronary arteries, and so more tests and procedures were done afterwards to clarify things," he wrote. "Another possibility is that seeing disease in an artery leads the doctor to want to 'fix it' with an angioplasty or bypass, while a stress test result does not provide as dramatic a picture."
Hlatky added that he agreed with Schoepf that more outcome studies are needed that explore length of life, symptoms, quality of life, and quality-adjusted life-years "to judge whether the significantly higher spending and higher procedure rates are good for patients and provide value."
Speaking by telephone with AuntMinnie.com, Min, whose work has contradicted the study findings, called the JAMA data "intriguing," but added that contemporary observational data "don't appear to support these findings."
"As an example, for the prospective, multicenter, international CONFIRM registry, we identified a very low rate of downstream angiography from patients without significant coronary disease, and even among those with obstructing coronary artery disease we found that less than half were being referred for invasive angiography," he said.
It may be that the JAMA study findings "were true at an early stage in the evolution of current-generation CT, for example 2006 to 2008, and it may be that if they were to examine more contemporary claims their results may have been different," he said.
Based on these results, clinicians and policymakers "should critically evaluate the use of CCTA in clinical practice, based on studies of subsequent outcomes," the authors concluded.