Their study reviewed patients who came to the hospital between 2001 and 2012 with abusive head trauma. MRI and MRV were used to assess subdural hemorrhage, parenchymal abnormalities, and thrombosis.
"MRI gives a better soft-tissue resolution than CT and is also multiplanar with many different sequences, which help to differentiate a clot around the vessel from a clot at the end of a torn vessel," explained lead author Dr. Arabinda Kumar Choudhary, chair of the department of medical imaging. "Thrombosis within the distal end of the torn veins can also be better appreciated on MRI."
A total of 45 studies (62% males) were reviewed; subjects had a median age of 3 months. The review found 41 (91%) children with subdural hematoma.
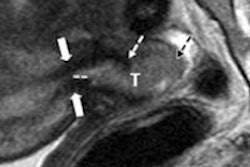
On MRV, 14 (31%) of the 45 cases had no evidence of venous compression, while the remaining 31 cases (69%) had imaging evidence of cortical vein and/or sinus compression. Evidence of direct trauma to the veins (lollipop sign) could be identified in 44.5% of cases, and there were no cases of cortical vein compression or lollipop sign without subdural hemorrhage, according to the researchers.
"One of the key arguments in the courts in the defense of abusive head trauma is that intracranial bleed happens because of primary thrombosis of the intracranial veins and sinuses and not from traumatic injury to the veins," Choudhary said. "The aim of our research is to demonstrate that thrombosis is present in abusive head injury, but it has a very distinctive appearance and is the result of primary injury to the vein with secondary thrombosis."
An inaccurate diagnosis of abusive head trauma could result in "devastating implications" and the possible separation of an infant from his or her family, a prison term for the child's caretaker, and significant medicolegal implications in the future. "At the same time, missed diagnosis of abusive head trauma can be fatal to the infant involved," he added.