Rheumatoid Arthritis:
View cases of rheumatoid arthritis
Clinical:
Rheumatoid arthritis is a common collagen vascular disorder that affects 1-2% of the general population [7,8]. The etiology of rheumatoid arthritis (RA) has not been established, but may be related to an immune reaction to some unknown antigen with an associated genetic predisposition. A majority of patients with RA are HLA-DR4 or DR1 (which are encoded on chromosome 6). No single test is diagnostic of the disorder. The criteria for the diagnosis of rheumatoid arthritis includes morning stiffness for at least 1 hour; arthritis (swelling) of three or more joints; arthritis (swelling) of the joints of the hands or wrists; symmetric arthritis; rheumatoid nodules; a positive rheumatoid factor; or the typical radiographic changes in the hands and wrists [4]. RF is a substance that agglutinates sensitized sheep RBC's. Approximately 85% of patients with RA are rheumatoid factor positive, and the RF titer correlates loosely with disease severity. Unfortunately, RF is not specific for RA as it may be identified in other infectious/inflammatory diseases. Pulmonary disease in patients with rheumatoid arthritis nearly always follows the onset of skeletal disease, although it may rarely be the presenting abnormality in these patients. HLA-DR4 positive patients have an increased incidence of pulmonary manifestations.RA is most commonly diagnosed in adults aged 20-50 years [8]. Although RA is much more common in females (3:1) [7], pulmonary disease is most commonly identified in males (5:1). Affected patients are typically between the ages of 25-50 years and in nearly 50% of patients there is some form of extraarticular involvement [7]. Lung disease is the second most common cause of death, following infection [7].
Pulmonary manifestations include:
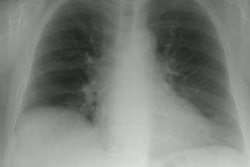
Pleural disease is the most common intrathoracic manifestation of rheumatoid arthritis [3,7]. Up to 5% of patients with RA have radiographic evidence of a pleural effusion sometime during the course of their disease, however, only about 20% of affected patients will be symptomatic [3]. Pleural manifestations are more common in men and in patients with longstanding severe arthritis [3]. Effusions are typically small, unilateral, and associated with periods of active arthritis [3]. The effusion typically resolve over weeks to months with treatment of the active arthritis (but they can last longer) [3]. The effusion is characteristically exudative with a low glucose level (less than 50 mg/dl in 75% of patients), low white cell count (less than 5000/mm3), and a low pH (less than 7.2) [3].
The interstitial lung disease associated with rheumatoid arthritis is histologically indistinguishable from idiopathic pulmonary fibrosis (UIP), unlike other collagen vascular diseases in which NSIP predominants [7]. RA patients that develop ILD uncommonly progress to respiratory failure [3]. A lower lobe predominance is also characteristic. Males are affected more than females. Radiologically detectable disease occurs in about 10-30% of rheumatoid patients (other authors indicate that the presence of clinically significant ILD in patients with RA is about 5% [7]). Arthritis precedes development of interstitial lung disease in 90% of cases [3], and 90% of patients have a positive serum rheumatoid factor. On HRCT findings include sub-pleural nodules (3-30mm) in up to 22% of patients, pseudoplaques, areas of ground glass attenuation (14%), fine reticular interstitial disease with a basilar predominance, and later honeycombing [1].
The presence of necrobiotic nodules in the lungs is usually associated with the presence of cutaneous nodules (to which they are histopathologically identical [8]). They are found in fewer than 1% of RA patients (they are also rarely associated with inflammatory bowel disease [9]). The nodules often develop concomitantly with joint disease, but they may precede the onset of arthritis. The pulmonary nodules are more frequently seen in patients with advanced stages of the disease, but they do not reflect disease activity [8]. Affected patients are typically asymptomatic [8], although cough, dyspnea, and hemoptysis have been described as presenting symptoms. A rare association is Caplan syndrome, in which multiple necrobiotic nodules develop in RA patients with coal workers pneumaconiosis [9].
The nodules are more common in men and can range in size from 0.5 to 7.0 cm [3]. Affected patients are also usually smokers and have high rheumatoid factor titers [7]. The nodules do not calcify, are usually peripheral/subpleural, adjacent to interlobular septa, and have an upper and mid-lung predominance [3,7,8,9]. Cavitation may be identified in up to 50% of nodules [3]. The nodule is often centered on a necrotic inflamed blood vessel, suggesting that vasculitis may be the initial insult. However, other authors note that patients treated with methotrexate have increased formation of lung nodules- this is felt to be related to activation of adenosine A1 receptors by methotrexate which leads to enhanced cellular fusion and formation of multi-nucleated giant-cell granulomas [9].
The clinical course of patients with rheumatoid pulmonary nodules is usually benign. The nodules may resolve spontaneously, recur, or develop at one site while resolving in another [3]. Methotrexate can result in paradoxical enlargement [9]. Pneumothorax secondary to rupture of a subpleural cavitary rheumatoid nodule is an exceedingly rare potential complication [8].
Caplan's syndrome is characterized by rheumatoid arthritis with pulmonary rheumatic nodules in coal workers typically with preexisting mild pneumoconiosis [3]. The nodules typically measure between 0.5 to 5 cm in size and may cavitate.
Drugs used in the treatment of rheumatoid arthritis have also been associated with the development of interstitial lung disease. Drug induced interstitial pneumonitis can occur in 5% to 10% of patients treated with methotrexate. It characteristically elicits no eosinophilic response and will resolve when the drug is discontinued [3]. Interstitial pneumonitis is also associated with gold therapy. The pneumonitis also usually resolves when the drug is stopped [3].
Systemic vasculitis in patients with rheumatoid arthritis is rare [3]. The most common presenting symptom is hemoptysis in the setting of a pulmonary-renal syndrome. Treatment usually involves corticosteroids and cyclophosphamide [3].
Airway disease has only recently been described in patients with RA. Bronchiectasis and bronchiolectasis have also been identified in up to 30% of patients [2,7]. Bronchiolitis obliterans [3], constrictive bronchiolitis, and follicular bronchiolitis [5] have also been described.
REFERENCES:
(1) Diseases characterized primarily by linear and reticular opacities. In: High Resolution CT of the Lung, 2d ed. Ed: Webb WR. 109-148 (p.122)
(2) Radiology 1994; 193:375-382
(3) J Thorac Imaging 1992; Shannon TM, et al. Noncardiac manifestations of rheumatoid arthritis in the thorax. 7: 19-29
(4) N Engl J Med 1990; Harris ED. Rheumatoid arthritis: Pathophysiology and implications for therapy. 322: 1277-1289 (Review. No abstract available.)
(5) Society of Thoracic Radiology Annual Meeting 2000 Course Syllabus; Erasmus JJ. Pulmonary drug toxicity: Pathogenesis and radiologic manifestations. 65-68
(6) Radiology 2004; Tanaka N, et al. Rheumatoid athritis-related
lung diseases: CT findings. 232: 81-91
(7) Radiographics 2012; Capobianco J, et al. Thoracic
manifestations of collagen vascular diseases. 32: 33-50
(8) Radiology 2017; Chaudhry AA, et al. Case 238: Spontaneous
pneumothorax secondary to intrapulmonary necrobiotic rheumatoid
nodule. 282: 602-608
(9) Radiographics 2020; Naeem M, et al. Noninfectious granulomatous diseases of the chest. 40: 1003-1019