Radionuclide Therapy for Tumors
Phosphorus-32 sodium phosphate (Soluble):
Chemistry and Pharmacology:
The agent is "clear" and is given intravenously. It can be given orally, but variable absorption (40-80% depending on the patients diet) may limit it's effectiveness [3]. P-32 has a physical half-life of 14.3 days and decays solely by beta emission to S-32 with a max energy of 1.71 MeV (Average 0.7 MeV) [5]. The mean range for the beta particle in tissue is 3 mm (max 8mm) [5]. Low energy bremsstrahlung radiation occurs, and can be used to assay the dose of the agent with a conventional dose calibrator or image the agents biodistribution following adminstration with moderate success.
Distribution
P-32 is taken up by most metabolically active tissues in the body, but about 85% of the administered dose localizes to bone because of its high inorganic phosphorous content (85% of total body phosphate is held within the skeleton [6]). P-32 is incorporated into the hydroxyapatite molecule [3]. The ratio of phosphorous uptake in tumorous bone relative to normal bone is about 2-5:1 [2,6]. The bone receives about 100 to 450 rads per 7 mCi dose (red marrow absorbed dose approaches 6.5 mGy/MBq [6]). The liver also accumulates the agent due to its high phosphorous turnover rate. Although 90% of the agent is filtered by the glomeruli, 85-90% is reabsorbed primarily in the proximal tubule. About 5 to 10% of the injected dose is excreted in the urine in the first 24 hours and about 20% during the first week. The whole body dose is about 70 rads/7mCi.
P-32 in the Treatment of Painful Bone Metastases:
Patients eligible for therapy are those that are not responsive to the usual analgesic medication. Their pain should emanate from the areas shown to be abnormal on the bone scan. Pain not arising from these sites should not be considered for this treatment [1]. The usual dose of the agent is 7 mCi (<12 mCi). P-32 is effective in palliating bone pain in 50-70% of patients with bone mets (25% have good response and 50% a partial response). Breast cancer patients had a slightly better response compared to those with prostate cancer. Pain palliation generally occurs within 14 days [5] and the mean duration of pain relief in about 5 months.
The main disadvantage of P-32 therapy is dose-limiting myelosuppression [6] which can be seen in 30-100% of treated patients. This pancytopenia is dose dependent and tends to nadir between the 4th and 5th weeks post therapy. When administered in doses less than 12 mCi, it is unlikely that significant granulocyte reduction (< 1000) will occur or that transfusion will be required. Recovery is usually seen by 6 to 7 weeks. A transient flare of increased pain is seen in 10%. There is no dose-response relationship between the dose of P-32 and pain relief. P32 may be as safe and as effective as Sr89 for the palliation of painful bone metastases and is much less expensive [1,3].
P-32 Treatment of Polycythemia Vera:
PCV is characterized by an overproduction of red cells, often with increased numbers of white cells and platelets as well. Without treatment the median survival is less than 2 years. The three main forms of therapy are phlebotomy, chemotherapy, and P-32. P-32 therapy appears to be best reserved for patients over the age of 75 years or who have failed other treatments.
Typical dose is 4 to 5 mCi I.V., with a majority of patients returning to normal blood chemistries by 4 to 6 weeks. If no response is seen by 3 months (Hct remains above 47 percent or continued phlebotomy required), retreatment with 5 mCi can be performed. This regimen may be repeated for one year, at which time if there has been no response to treatment, another mode of therapy should be instituted. The remission may last for years.
Although the risk of developing myelofibrosis with myeloid metaplasia is unlikely related to therapy, there is an increased incidence of leukemia (up to 10 to 20%) in patients with PCV treated with P-32 compared to those treated by phlebotomy alone. Leukemia has been associated with doses over 12 mCi. Nonetheless, median survival following P-32 treatment is10 to 15 years, compared to 7 to 8 years with phlebotomy.
Colloidal Chromic Phosphate P-32 Suspension:
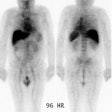
Primarily used for the treatment of serosal implants. The objective of the treatment is to prevent recurrent malignant effusions. The agent is "green" in color and should not be administered I.V. (Since it is a colloid, it would localize to the liver). The particle size is between 0.1 to 0.3 microns. Doses are about 15-20 mCi for intraperitoneal administration, 10 mCi for intrapleural, and 5 mCi for pericardial. A preliminary intraperitoneal Tc-sulfur colloid scan is performed to evaluate for the presence of loculated fluid which is a contraindication to the treatment. Following injection of the agent, it is important to turn the patient frequently to obtain a homogeneous distribution and a bremsstrahlung scan should also be obtained. About 90% of the administered dose plates out on serosal surfaces with ablation of serosal and lymphatic deposits (there is about a 50-80% response rate- i.e.: no recurrent fluid). The treatment has little effect on bulky tumors. There are no adverse hematologic effects. Complications of the therapy are usually minor (nausea, abdominal pain, vomiting, diarrhea, and low grade fever) and can be seen in up to 20% of treated patients. Major complications such as bowel obstruction or perforation may also occur in about 1% of patients, however, it is often difficult to say if this is the result of the treatment or a complication of the underlying disease [4]. Enhanced therapeutic responses can be seen if the treatment is given in conjunction with cis-platin chemotherapy [4].
REFERENCES:
(1) J Nucl Med 1999; Nair N. Relative efficacy of P32 and Sr89 in palliation in skeletal metastases. 40: 256-261
(2) J Nucl Med 2001; Serafini AN. Therapy of metastatic bone pain. 42: 895-906
(3) Semin Radiat Oncol 2000; Silberstein EB. Systemic radiopharmaceutical therapy of painful osteoblastic metastases. 10: 240-249
(4) J Nucl Med 1995; Jan.: p.29-36
(5) J Nucl Med 2004; Pandit-Taskar N, et al. Radiopharmaceutical therapy for palliation of bone pain from osseous metastases. 45: 1358-1365
(6) J Nucl Med 2005; Lewington VJ. Bone-seeking radionuclides for therapy. 184: 38S-47S