Bone Imaging
Trauma:
Fractures: General findings
Bone scintigraphy is a very sensitive exam for the detection of
acute fractures [5]. About 80% of bone scans will show increased
activity at a site of fracture by 24 hours, and 95% by 72 hours,
although older (over 75 y) and debilitated patients may not show
activity for several days to as much as 2 weeks.
There are generally 3 phases identified when evaluating fractures:
There is increased flow and blood pool activity with diffuse and somewhat poorly defined increased delayed activity about the fracture site which is wider than the fracture line. Gallium uptake at acute fracture sites is usually increased as well. Mildly increased uptake of In-111 WBC's at the fracture site is present in up to 40% of acute uncomplicated fractures and may be associated with callus formation or adjacent myositis ossificans. Significant accumulation of white blood cells at the site of a healing fracture DOES NOT generally occur (seen in only 4% of cases) unless there is a complicating osteomyelitis.
Flow and blood pool abnormalities diminish considerably and delayed activity becomes more localized (focal at the fracture site) and intense.
A gradual decline in activity occurs over time with about 65% of exams normalizing by 1 year, and 90% becoming normal by 2 years. The minimum time for normalization of activity is 6 months after the fracture [7]. Persistent activity can be seen if healing has not produced normal anatomic alignment in weight bearing areas due to continued biomechanical stress and remodeling. Non-union occurs when there is failure of the fracture site to heal by 6 to 8 months following the injury. The tibia is the most frequent site of non-union. Non-union may occur secondary to an inadequate blood supply, osteoporosis, or infection. Two types of non-union have been described: reactive and atrophic.
Suspected wrist fracture:
In the evaluation of suspected wrist fracture, up to 45% of patients presenting with continued pain 10-14 days after injury and normal radiographs can be found to have a fracture on skeletal scintigraphy [5].
Reactive Non-union:
Characterized by persistent intense or normal uptake at the fracture site (80%). This bone has potential for healing (i.e.: evidence of metabolic activity) and these fractures tend to show significant improvement following electrical stimulation. Indium labeled WBC's are probably more reliable for detecting infection at the site of reactive non-united fractures, as gallium will also accumulate at these sites. It is not possible to distinguish a reactive non-union from a delayed union.
Atrophic Nonunion:
Appears as a photon deficient band between the fracture ends, which themselves may have more or less activity. This group of non-united fractures is usually not responsive to percutaneous electric stimulation.
Child Abuse:
Fractures of the femur or humerus, especially in children less than 1 years of age are very suspicious for child abuse. In the setting of the battered child, metaphyseal fractures near the growth plates, healed fractures, and skull fractures may be very difficult to visualize scintigraphically. It is best to perform a radiographic survey initially, and follow with scintigraphy if more information is required. Scintigraphy does have increased sensitivity for the detection of rib fractures compared to plain radiographs [1].
Vertebral Compression Fracture:
Regarding vertebral compression fractures, as with other fractures, most elderly patients will have a positive bone scan by 48 hours, however, the exam may not become positive for 3 to 7 days in up to 5-10% of patients. By 1 year, about 60% of compression fractures will normalize and 95% will become normal by 3 years. When multiple fractures are present in different stages of healing, osteoporosis is the most likely diagnosis. Multiple myeloma may occasionally mimic this appearance.
Stress/Insufficiency Fractures:
Stress fractures occur due to repetitive forces/cyclical loading
placed on normal bone [21]. Bone adapts to stress with internal
remodeling that will strengthen the bone to withstand the
particular stress [3]. During remodeling, there is a period when
resorption exceeds replacement of bone which temporarily weakens
the cortex [3]. Microfractures can result at these sites of
resorption if the stress is continually applied during this period
(when the rate of accumulated microdamage outpaces the ability of
the bone to regenerate through the normal remodeling process
[21]). Gross fracture may result if these microfractures are not
permitted to heal. Insufficiency fractures result from normal or
physiologic loads placed on bone with deficient elastic
resistance. Up to 40% of patients with stress fractures can be
asymptomatic [5]. Most stress fractures involve the tibias and
more than one stress fracture can be found in up to 87% of
patients [5].
The most common stress fractures are low-risk fractures of the
posteromedial tibia, the calcaneus, the third and fourth
metatarsals, and the medial femoral neck [21]. High risk fractures
include the superolateral femoral neck, the patella, the anterior
tibial cortex, the medial malleolus, the talar neck, the dorsal
navicular cortex, the proximal metaphysis of the 5th metatarsal,
and the sesamoids of the great toe [21]. Additionally, proximal
femoral stress fractures with a fatigue line greater than 50% of
the width of the femoral neck, or fractures with any evidence of
displacement should be considered high risk [21].
Radiographically, stress fractures appear as a lucent fracture line, focal sclerosis due to endosteal callous formation, a periosteal reaction, or as an external callous.
Bone scan is much more sensitive than plain film for diagnosing stress fractures [5]. More than 80% of stress fractures will not be evident on intial radiographs, while the sensitivity of bone scan for the diagnosis of stress fracture approaches 100% [3]. On bone scan stress fractures usually appear as solitary, focal, fusiform areas of increased tracer activity generally lasting for 10 to 12 weeks. Increased flow (for up to 3 to 4 weeks after onset of pain) and increased blood pool (for 6 to 8 weeks) activity may also be seen. The scintigraphic abnormality often precedes the radiographic changes by 1 to 2 weeks.
Stress fractures can be classified into 4 grades according to the dimension of the scintigraphic abnormality [5].
Grade I is a small, focal, ill-defined lesion with mildly increased cortical activity.
Grade II is larger than grade I, well-defined, focal, elongated and moderately increased activity confined to the cortex.
Grade III is a focal, wide, fusiform lesion with highly increased activity involving the cortico-medullary region (extending less than half-way through the width of the bone).
Grade IV is a focal, wide, extensive lesion with intensely increased activity in the transcortico-medullary region (extending more than half-way through the width of the bone).
The metatarsals and the posterior medial cortex of the tibia are the most common locations for stress fractures. Stress fractures of the tarsal navicular bone are uncommon, but can produce foot pain in athletes. They most commonly involve the central one third of the proximal dorsal margin of the tarsal navicular bone. During evaluation of the symptomatic area, asymptomatic sites of increased tracer activity can be found in up to 40% of athletes [3]. These secondary abnormalities likely reflect uptake related to functional adaptive bone remodeling [3]. Asymptomatic abnormalities are unlikely to progress to stress fracture when they are characterized by generalized increased activity in the feet or along the posterior tibia [3]. Asymptomatic focal abnormalities within the anterior tibia or femoral neck should not be ignored as stress fracture in these regions can be associated with significant morbidity [3].
Tracer uptake in the femoral neck region can often be described in one of three patterns-
1) Focal uptake along the upper portion of the femoral neck just below the femoral head- this pattern of uptake is suggestive of a herniation pit [6].
2) Focal uptake along the upper portion of the femoral neck more towards the greater trochanter- this pattern is seen with a tension type stress fracture [6]. This type of stress fracture is associated with an increased risk for a displaced femoral neck fracture and it may require operative stabilization [6]. This type of stress fracture is more common in the elderly [6].
3) Focal uptake along the inferior aspect of the femoral neck towards the lesser trochanter- this pattern of uptake is associated with a compression type stress fracture which is more stable and can be treated conservatively. This type of stress fracture is more common in young adults [6]. SPECT imaging is much more sensitive than planar imaging for the detection of femoral neck stress fractures and can demonstrate fractures in patients with normal planar imaging [10].
Stress fractures of the femur can occur in athletes and military
recruits ands most commonly involve the medial cortex of the
proximal femur [11]. This area of the proximal femur is
susceptible to stress fracture because of the origin of the vastus
medialis and insertion of the adductor brevis [11]. Insufficiency
fractures of the proximal femur in the elderly usually involve the
lateral cortex [11].
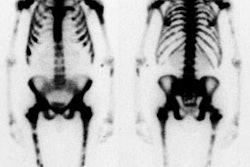
In the sacrum, stress fractures are associated with osteoporosis or prior radiation therapy to the pelvis (an insufficiency fracture) [10]. The osteoporotic sacrum develops a characteristic fracture with fracture lines running vertically through the left and right sides of the bone just medial to the SI joints, in conjunction with a transverse fracture just below the level of the SI joints. The fractures appear as a hot, geographic lesions confined to the sacrum and often have a characteristic "butterfly" or "Honda sign" appearance. Plain film are typically normal, but may show a sclerotic lesion in sacral ala.
Shin splints (stress periosteal reaction) are due to abnormal movement of the either the soleus muscle tendon complex or posterior tibialis muscle with disruption of Sharpey's fibers which produces a periostitis type lesion. Shin splints are characterized by abnormal linear (not focal) uptake of tracer along the posteromedial tibial cortex. A similar problem involving the tibialis anterior muscle has been suggested for abnormal activity along the anterior tibial cortex. Shin splints have not been demonstrated to progress to stress fractures. Shin splints are mainly treated with anti-inflammatory drugs [5].
Tendonitis may occasionally be detected on bone scan. Plantar fasciitis shows increased activity at the calcaneal tubercle. Patellar tendonitis at the inferior pole of the patella. Achilles tendonitis will show focal increased activity at the Achilles insertion on the posterior calcaneus (Differential diagnosis includes retrocalcaneal bursitis which usually appears more diffuse and less focal). Medial epicondylitis demonstrates focal increased activity over the medial humeral epicondyle at the insertion of the pronator flexor group.
Atypical femoral
neck fracture/Bisphosphonate associated fracture:
Bisphosphonate therapy is used for the treatment of osteoporosis.
There are four commonly used agents- alendronate sodium (Fosamax-
most commonly used agent), risedronate, ibandronate, and
zoledronate [15]. Biphosphonate therapy acts by the inhibition of
osteoclast function and maturation and induction of osteoclast
apoptosis- thereby reducing bone resorption [12,15,21]. Although
this can lead to increased bone mineral density, the resulting
suppression of bone turnover and bone remodeling can lead to
atypical skeletal fragility (biphosphonates limit the native
repair mechanisms of bone and microfractures can place the patient
at increased risk for long-bone fractures) [12,17].
Patients receiving bisphosphonate therapy have been shown to be
at increased risk for insufficiency fractures of the proximal
femur [11,12] - especially atypical fractures of the lateral
cortex which are oriented transversely [21]. Most fractures occur
as a result of minimal or low-impact trauma, although a lesser
number of patients experience a spontaneous fracture (this is
referred to as an atypical fracture) [13,17]. The presence of a
proximal femoral diaphyseal fracture after low energy trauma
should raise suspicion for long-term bisphosphonate use (>3
years) [11]. Between 50-60% of patients experience prodromal
sumptoms of pain in the leg or groin before the fracture [13].
However, fractures have been observed in up to 2% of asymptomatic
patients [18]. The incidence of insufficiency fracture of the
femoral shaft in patients receiving continuous bisphosphonates has
been reported to be 1 per 1000 annually [11]. Patients with
alendronate fractures tend to be active women, typically in their
late 50's and early 60's, who have been taking the agent for at
least 3 years [18].
Prior to actual fracture, the plain film can show focal cortical
thickening (or thickening with a thin perpendicular lucency- "the
dreaded black line") along the lateral margin of the proximal of
mid femur and this area will demonstrate focal tracer uptake on
bone scan [12,13,15,17]. There can be a similar finding involving
the contralateral femur in up to 53% of patients [17]. The
fracture most commonly affects the subtrochanteric region of the
femoral shaft (close to the lesser trochanter) with a transverse
or short oblique orientation to the fracture line [15,17].The
fracture is generally non-comminuted [15]. A "medial spike"-
defined as a sharp medial cortical projection arising from the
distal (but sometimes proximal) fracture fragment- has also been
described [15].
Treatment for atypical femoral stress fracture may include
cessation of anti-resporptive treatment, possible supplementation
with calcium and vitamin D, consideration for therapy with bone
forming agents (such as teriparatide), and screening of the
contralateral femur (up to 44% of patients demonstrate a fracture
in the contralateral femur at presentation or subsequently) [21].
Spondylolysis and low back pain evaluation:
Skeletal scintigraphy is highly sensitive for detecting stress-induced changes in bone and is an important part of the evaluation of the young athlete with low back pain [8].
Spondylolysis is felt to represent a fatigue type fracture of the
par interarticilaris of the vertebrae that occurs secondary to
repetitive minor trauma (generally hyperextension) [4]. Most
patients present with either acute or chronic pain. Skeletally
immature individuals are prone to develop spondylolysis, with the
highest rate observed during the teenage growth years [16]. It can
be found in as many as 47% of adolescent athletes with low back
pain [16]. The sports most commonly associated with spondylolysis
are gymnastics, diving, ballet, and contact sports such as
football, hockey, and lacrosse [4]. The injury can be observed in
11% of young femal egymnasts, 20% of college football players, and
28% of wrestlers [16].
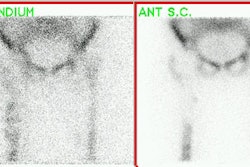
Approximately 90% of pars defects occur at the L5 level [4]. With a unilateral pars defect (30% of cases), sclerosis, thickening, and enlargement of the contralateral lamina and pedicle can occur (Wilkinson's syndrome) [4]. These findings are most likely the result of stress related changes. SPECT imaging is more sensitive than planar studies and will detect abnormalities in about one third of individuals with normal planar exams [4]. Spondylolysis produces little or no abnormality on blood pool images. Delayed images will show focal tracer accumulation in the region of the pars interarticularis. Even mild localizations of tracer in this location are significant and deserve therapy [4]. With response to treatment, SPECT findings should gradually diminish over 6 months to 1 year [4]. A normal SPECT exam implicates a cause other than bone pathology as the cause of the patients pain [4]. In patients with a known radiographic defect, a normal scan indicates that the lesion is quiescent and may represent non-union or an incidental finding. SPECT imaging of the cervical and upper thoracic spine may be disappointing due to spinal curvatures, the relatively smaller size of the vertebral bodies and disc spaces, and the larger distances required for the detector to clear the shoulders in a circular orbit.
Other causes of low back pain in children and young adults include:
Spinal process apophysitis produces uptake of tracer along the
lumbar spinous process and is due to a hyperextension overuse
injury. Lumbar interspinous bursitis (Baastrup disease) is
believed to be related to excessive lordosis which results in
mechanical impingement on adjacent spinous processes (L4-5 is most
commonly affected) [19]. The impingement can occur at one or more
spinal levels [19]. Patients tend to be older with disk bulges,
central canal stenosis, and anterolisthesis, but can also occur in
young athletes due to repetitive hyperextension and hyperflexion
[19]. Radiographs and CT typically demonstrate close approximation
or abnormal cortical contact, spinous process enlargement,
flattening, and sclerosis of the opposing spinous process cortical
surfaces [19,20]. SPECT will demonstrate focal tracer uptake in
opposing spinous processes [19]. PET can demonstrate
mild-to-moderate FDG uptake [20]. MR imaging will demonstrate
interspinous fluid [19].
Lumbosacral transitional vertebra: A lumbosacral transitional vertebra is a common anomaly characterized by a large transverse process that follows the contour of the sacral ala and forms a non-ossified articulation with the sacrum [8]. The anomalous vertebra is commonly referred to as a "sacralized" L5 or a "lumberized" S1 on the basis of the number of non-rib bearing vertebrae [8]. Lumbosacral transitional vertebrae can alter the biomechanics of weight transfer at the affected spinal segment [8]. Bertolotti syndrome refers to low back pain in patients with a transitional vertebral body and increased tracer uptake along the transverse process pseudoarthrosis of a transitional vertebrae which is indicative of stress change [8,19]. This finding can be seen in about 80% of patients with a transitional vertebra and low back pain [8]. SPECT images are generally superior to planar scintigraphy for demonstrating tracer uptake (nearly 60% of abnormalities will only be evident on SPECT images) [8]. MRI is often not revealing in these cases [8]. Treatment may include use of a lumbosacral orthosis, physical therapy to stretch and stabilize the spine, and sport-specific training to limit expose to the mechanism of injury [8]. Corticosteroid injections may be required in rare cases and in very rare instances, surgical fusion or resection of the articulating transverse process can be performed [8].
Slipped Capital Femoral Epiphysis:
In the absence of avascular necrosis the bone scan findings in slipped capital femoral epiphysis are nonspecific and consist of mildly increased activity about the hip and widening and blurring of the growth plate activity.
Facet Syndrome:
The posterior spinal compartment syndrome is a controversial disorder related to the lumbar facet joints that can produce both local and radiating pain associated with poorly defined or absent neurological findings. Although degenerative changes of the facets are commonly seen in these patients, there is no reported correlation of symptoms with plain film or CT evidence of such changes. SPECT bone imaging will usually detect an abnormality (sensitivity 100%), but the exam suffers from a lack of specificity (70%). Nonetheless, a normal exam confirms the absence of facet syndrome, and the examination can also demonstrate other, non-facet related lesions [2].
Intervertebral Disc Herniation:
An acute herniated nucleus pulposus will not cause any changes on a bone scan until there has been excessive stress placed on the adjacent vertebrae. When this occurs, increased activity can be seen in the end-plates of the vertebral bodies on either side of the of the disc.
Schuermann's Disease:
The disorder is relatively uncommon, occurring in 3 to 5% of adolescents [4]. It is characterized by vertebral body wedging, kyphosis, end-plate irregularity, and herniation of disc material [4]. The diagnosis is established when the radiographs demonstrate anterior wedging greater than 5 degrees with involvement of 3 or more contiguous vertebral bodies and a structural kyphosis of greater than 40 degrees. It is believed to be related to repeated trauma with vertical forces causing the nucleus pulposus to migrate through the weak portion between the ring apophysis and the vertebral end-plate [4]. Schmorl's nodes- herniation of the disc into the vertebral body end-plate, are also seen in about 25% of cases. Bone scan may show a slight increase in tracer accumulation along the end-plate regions. This abnormality will be more apparent on SPECT images. Nonetheless, the diagnosis is made radiographically [4].
Also referred to as posterior impingement syndrome the condition is caused by repetitive plantar flexion leading to compression of bone and soft tissues at the posterior ankle [14]. The condition is commonly seen in ballet dancers and soccer players [14]. Predisposing conditions include an os trigoum, a prominent lateral talar process (Stieda process), a shelf-like superior prominence of the calcaneal tuberosity, and a posterior intermalleolar ligament [14]. Patients develop symptoms of pain and tenderness along the posterior ankle that is exacerbated on plantar flexion or dorsiflexion [14]. On bone scan, focal increase tracer uptake can be seen in the region of the posteior ankle joint or in the os trigonum.
REFERENCES:
(1) Semin Nucl Med 1993; Conway JJ, et al. The role of bone scintigraphy in detecting child abuse. 23(4):321-33. Review.
(2) J Nucl Med 1995; Holder LE, et al. Planar and high-resolution SPECT bone imaging in the diagnosis of facet syndrome. 36(1):37-44
(3) J Nucl Med 2001; Drubach LA, et al. Assessment of the clinical significance of asymptomatic lower extremity uptake in young athletes. 42: 209-212
(4) Semin Nucl Med 1993; Sty JR, et al. Spine pain in children. 23: 296-320
(5) J Nucl Med 1987; Zwas ST, et al. Interpretation and classification of bone scintigraphic findings in stress fractures. 28: 452-457
(6) J Nucl Med 2002; Sopov V, et al. Clinical spectrum of asymptomatic femoral neck abnormal uptake on bone scintigraphy. 43: 484-486
(7) Radiographics 2003; Love C, et al. Radionuclide bone imaging: an illustrative review. 23: 341-358
(8) J Nucl Med 2003; Connolly LP, et al. Skeletal scintigraphy of young patients with low-back pain and a lumbrosacral transitional vertebra. 44: 909-914
(9) AJR 2005; Groves AM, et al. 16-MDCT in the detection of occult wrist fractures: a comparison with skeletal scintigraphy. 184: 1470-1474
(10) AJR 2008; Kwon JW, et al. Pelvic bone complications after
radiation therapy of uterine cervical cancer: evaluation with MRI.
191: 987-994
(11) AJR 2010; Porrino, Jr. JA, et al. Diagnosis of proximal femoral insufficiency fractures in patients receiving bisphosphoate therapy. 194: 1061-1064
(12) AJR 2010; Chan SS, et al. Subtrochanteric femoral fractures in patients receiving long-term alendronate therapy: imaging features. 194: 1581-1586
(13) AJR 2010; Rogers LF, Teljanovic M. FDA staement on relationship between bisphosphonate use and atypical subtrochanteric and femoral shaft fractures: a considered opinion. 195: 563-566
(14) AJR 2010; Donovan A, Rosenberg ZS. MRI of ankle and lateral
hindfoot impingement syndromes. 195: 595-604
(15) AJR 2011; Rosenberg ZS, et al. Bisphosphonate-related
complete atypical subtrochanter femoral fractures: diagnostic
utility of radiography. 197: 954-960
(16) Radiographics 2012; Jaimes C, et al. Taking the stress out
of evaluating stress injuries in children. 32: 537-555
(17) AJR 2012; Png MA, et al. Bisphosphonate-related femoral
periosteal stress reactions: scoring system based on radiographic
and MRI findings. 198: 869-866
(18) AJR 2012; La Rocca Vieira R, et al. Frequency of incomplete
atypical femoral fractures in asymptomatic patients on long-term
bisphosphonate therapy. 198: 1144-1151
(19) Radiographics 2015; Trout AT, et al. Spondylolysis and
beyond: value of SPECT/CT in evaluation of low back pain in
children and young adults. 35: 819-834
(20) Radiographics 2016; White ML, et al. Specturm of benign
articular and periarticular findings at FDG PET/CT. 36: 824-839
(21) Radiographics 2018; Marshall RA, et al. Imaging features and
management of stress, atypical, and pathologic fractures. 38:
2173-2192