Pharmacologic Stress Cardiac Imaging
Pharmacologic stress can be performed in patients that are unable to perform adequate exercise as a result of orthopedic or cardiopulmonary limitations [48]. Pharmacologic stress can be performed using either vasodilator agents (such as dipyridamole or adenosine) or dobutamine. Patients with reversible defects on pharmacologic stress exams have a higher cardiac event rate than similar patients with exercise stress (about 11% versus 5.6%) [38]. Patients with normal pharmacologic vasodilator stress SPECT exams have a generally good prognosis (annual risk of cardiac death or infarction of 1.3%-3.9%)- however, this is worse than the event rate in patients with normal exercise stress exams (which is less than 1%) [28,35,38,42,73]. This has been felt to be related to a greater degree of co-morbid conditions in patients that are selected for pharmacologic stress [38]. Typically, patients selected for pharmacologic stress are older and have a higher prevalence of cardiac and non-cardiac co-morbidities such as hypertension, diabetes, previous MI, and previous revascularization procedures [38,121]. The inability to perform any level of exercise during a MPI exam has been shown to be associated with a high mortality risk from both cardiac and non-cardiac death [121]. Even within propensity-matched cohorts, patients with pharmacologic stress have a three fold higher annualized event rate and nearly twice the mortality rate compared to patients with normal exercise stress imaging [73,122].
The presence of ischemic changes on ECG during pharmacologic stress is uncommon (between 1% to 7% of patients) [28,29] and is generally found in combination with reversible perfusion defects on perfusion imaging [42]. During vasodilator stess, the phenomenon is felt to be the result of a "coronary steal" and may be associated with the presence of multivessel coronary artery disease [42]. It is postulated that the pharmacologic vasodilatation produces less vasodilatation in vessels that have fixed stenoses [42,51]. Meanwhile, the resistance in normal coronary vessels will drop and this can cause blood flow to be diverted away from collateral vessels supplying vascular beds distal to diseased vessels with a critical stenosis [42,51]. This decrease in perfusion in the diseased vessel (which is collateral dependent) then leads to the development of ischemia [42]. Ischemic ECG changes noted during pharmacologic stress is a marker for increased cardiac event rates [42]. Patients that develop ECG evidence for ischemia with vasodilator stress should be further evaluated even if the SPECT images are normal [29]. In patients with normal pharmacologic stress images, the presence of ischemic ECG changes is associated with a higher risk for subsequent cardiac events (4%-7.5% at one year) [28,29]. Similar to vasodilator stress, the presence of ischemic ECG changes during dobutamine infusion also carries a higher risk for subsequent cardiac events (about 4% annual risk) [42].
Advantages
- Provides a standardized, consistent stress independent of patient endurance. A pharmacologic stress exam is likely to be more sensitive than a submaximal exercise scan for the detection of CAD.
- Not affected by antianginal drugs
- Greater increase in coronary flow than exercise stress (up to 4ml/min./gm which is 4 to 6 times baseline)
Drawbacks:
- Myocardial extraction of Tc-99 perfusion agents (tetrofosmin, sestamibi, and to a lesser extent thallium) is not linear during adenosine or dipyridamole induced hyperemia [19]. At higher flow rates (greater than 2 times baseline [2.5 to 3.0 mL-min-1 - gm-1]), there is decreased tracer extraction [19,47]. This decreased extraction results in underestimation of flow heterogeneity and can potentially result in underestimation of myocardial ischemia [19].
- Vasodilator pharmacologic stress will detect abnormalities in flow reserve [55]. Unfortunately, in patients with CAD, coronary vasodilator reserve is often abnormal, even in territories supplied by non-critical stenoses thereby reducing the heterogeneity of flow between normal and abnormal zones and limiting the ability to delineate the presence of multivessel CAD [55].
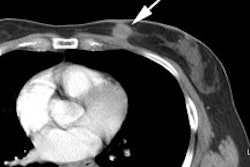
- Increased subdiaphragmatic gut
activity compared to exercise stress [86]: High
subdiaphragmatic count activity can affect image
interpretation by: 1- creating a ramp filter artifact that
result sin apparent decreased myocardial activity in the
adjacent walls; 2- scattering photons into the adjacent walls
artificially increasing the apparent count activity; 3- by
artificially increasing counts in one segment, other segments
may appear relatively hypoperfused; and 4- by resulting in
image normalization errors between stress and rest images
[86].
Indications for pharmacologic stress:
- Patients who cannot exercise adequately for diagnostic purposes such as patients with peripheral vascular disease in whom claudication is the rate limiting factor for exercise. Perfusion defects can be missed or underestimated in patients with submaximal exercise stress.
- Left bundle branch block: Pharmacologic stress should not result in a reversible septal defect as the heart rate should not increase significantly.
- Fixed rate ventricular pacemakers: In paced patients, the ECG is not interpretable on standard tredmill testing [40]. Pharmacologic stress provides significant prognostic information in patients with permanent pacemakers and can identify patients at high risk for subsequent cardiac events [40].
- Pre-operative risk stratification
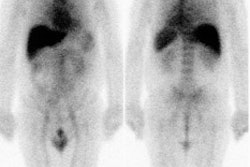
- Risk stratification in the early post myocardial infarction period [86]: During the early post-MI period, evidence of a reversible perfusion abnormality on the dipyridamole exam was the best predictor of future cardiac events in one study. [1]
Dipyridamole
Physiology & Pharmacology
Dipyridamole stress tests coronary flow reserve without increasing myocardial oxygen demands. Following injection, a radiotracer will preferentially go to areas perfused by normal coronary arteries, and proportionately less to areas supplied by stenotic vessels.
Dipyridamole acts indirectly via adenosine. Adenosine is normally produced by both the myocardial smooth muscle and endothelium [42]. Dipyridamole inhibits adenosine uptake by the vascular endothelium and alters red cell membranes thus preventing access to membrane bound adenosine deaminase which is the enzyme primarily responsible for adenosine degradation. This results in reduced degradation and increased blood levels of adenosine (it approximately doubles the circulating levels of adenosine). Adenosine then binds to A2a receptors which predominate in the cell walls of the coronary arteries which results in vasodilatation [42]. Adenosine is a potent arteriolar dilator and the resultant dilatation in the precapillary and arteriolar capillary beds results in 3 to 5 fold increase in coronary blood flow in normal vessels (hyperemic flows can range from 2 to 4 mL/min/gm) [30,69] (this frequently exceeds the augmentation in coronary flow by maximal exercise). Stenotic vessels with a limited coronary flow reserve demonstrate reduced responsiveness with relative flow reduction proportional to the degree of stenosis and a resultant defect on perfusion scintigraphy. Dipyridamole also usually causes a mild decrease in blood pressure and increase in heart rate [56].
Dipyridamole is eliminated with a biological half-life of 90 to 135 minutes, while the peak vasodilatory effects occur approximately 2 minutes following completion of a 4 minute infusion and the effect persists for 10-20 minutes following the infusion [30]. Adenosine levels remain elevated for 30 to 45 minutes despite a relatively rapid fall in dipyridamole plasma levels [8]. Because it acts indirectly, the coronary hyperemia induced with dipyridamole is less predictable than that seen with an adenosine infusion [86]. Dipyridamole is metabolized primarily in the liver with only minimal amounts excreted in the urine [8]. Prolonged pharmacologic activity could occur in the setting of hepatic insufficiency [8].
Technique
Prep: Caffeine, theophylline, and aminophylline are non-selective inhibitors of the adenosine receptor subtypes (adenosine receptor antagonists) [89]. Caffeine also indirectly stimulates adrenergic alpha 2 receptors to produce vasoconstriction [60]. All theophylline (xanthine) and caffeine containing medications should be held for 36 to 48 hours prior to the exam. There is large variation in individual caffeine metabolism- with a half-life ranging from 2 to 12 hours [60]. Cigarette smoking significantly decreases caffeine's half-life by the induction of liver enzymes, while patients with impaired liver function have reduced caffeine clearance [60]. Caffeine containing beverages should be avoided for 24 hours [25,60]. Caffeine can reduce the hyperemic effect of dipyridamole by as much as 70% [12]. When the effect of caffeine on the dipyridamole-induced changes in heart rate are examined, there is a consistent attenuation in the expected heart rate increase and the percent heart rate increase has been found to be inversely correlated with the plasma caffeine level [25,60]. Patients with a caffeine level of zero have a mean increase in heart rate of 18% [25]. A less than 5% increase in heart rate may indicate a blunted response to the dipyridamole infusion [25].
It is not necessary to discontinue dipyridamole prior to the examination, however, other authors recommend that this medication be stopped for 48 hours [48]. The patient should be NPO for 4 to 6 hours prior to the exam to decrease splanchnic activity and reduce the possibility of nausea and emesis. Antianginal medication may alter both resting and dipyridamole induced hyperemic myocardial perfusion [32]. Nitroglycerine results in a slight (10%) increase in perfusion to areas supplied by stenosed and non-stenosed arteries [32]. Metoprolol in standard doses also reduces both resting and hyperemic perfusion, but the effect is more pronounced following dipyridamole infusion (about 25% decrease in hyperemic perfusion) [32]. The potential clinical consequence is reduced diagnostic sensitivity [32]. Unless specified by the referring physician, beta-blockers and nitrates should be withheld for 24 hours prior to the exam [48]. Amlodipine does not seem to affect perfusion [32].
Under the typical protocol, dipyridamole is infused at a rate of 0.142 mg/kg/minute for 4 minutes through a large vein. (Approximately 0.56 mg/kg) Oral administration is not routinely used because it results in erratic absorption and GI upset. During the infusion BP & HR are monitored each minute, and the EKG continuously. Patients may typically have a mild elevation in heart rate (5 to 10 bpm) and a modest decrease in blood pressure (10-15 mmHg). The peak pharmacologic effects occur about 6 to 8 minutes following initiation of the infusion. Effects persist for 15 to 30 minutes, but may last as long as 60 minutes.
A myocardial perfusion agent is injected 2 to 4 minutes following completion of the infusion (typically at 7 minutes) or sooner if impressive hemodynamic side effects are noted. Aminophylline (an adenosine receptor antagonist) may be administered I.V. 3 to 4 minutes after thallium to abort the dipyridamole effects after radionuclide extraction. Vasodilator infusions yield higher cardiac uptake of thallium than exercise stress, but unfortunately, produce worse heart-to-background ratios due to higher blood thallium levels and vasodilatation of the splanchnic bed which can result in high infradiaphragmatic background activity. Walking, bicycle ergometry, or symptom-limited low level exercise beginning near the completion of the dipyridamole infusion and continued for 30 to 60 seconds following injection of the radiotracer, will help to reduce the amount of gut and liver activity, produce heart-to-background ratios similar to exercise alone (i.e. improve image quality), and help to decrease the incidence of non-cardiac side effects (such as vasodilator induced hypotension) [3,4,14,15,48,52]. Low level exercise can also improve ECG sensitivity for the detection of ischemia [15]. Concomitant beta-blocker therapy in patients undergoing symptom-limited dipyridamole stress testing adversely impacts the ability of MPI to risk-stratify (despite normal images these patient have a higher cardiac event rate) [52,53]. Hand grip exercise has been used, but it may not be very effective [5]. The measured thallium washout rate is slightly slower than that following exercise.
A drawback of dipyridamole imaging is that the standard dose utilized may not produce maximal coronary vasodilatation in up to 20% of normal subjects (near maximal coronary vasodilatation occurs more consistently with adenosine). Preliminary work indicates that higher doses of dipyridamole (0.84 mg/kg infused over 6 minutes) are safe and may increase the sensitivity of the thallium exam (although not statistically significant in this particular study and certainly controversial as the larger dose was not felt to enhance the coronary vasodilatory effect of the standard dose in another study [6]). Side effects, however, are more common with the higher dose (up to 79% of patients). The most frequently encountered side effect was chest pain (58%). [7]
Contraindications
NOTE: In patients taking oral dipyridamole (persantine, aggrenox) IV adenosine can result in profound heart block, however, IV dipyridamole can usually be safely adminisetered to these patients [86].Contraindications to the dipyridamole exam include:
- Allergy to dipyridamole
- Acute myocardial infarction within the preceding 48 hours
- Unstable angina
- History of severe bronchospasm, active bronchospasm, and
moderate or severe COPD (moderate COPD is COPD with a
significant reversible component- FEV1 30-39% of predicted with
bronchodilator response >15% or FEV1 40-100% predicted with a
bronchodilator response >30%; and severe COPD is FEV1 <30%
predicted) [86].
- Hypotension (Systolic BP < 90-100 mmHg): The average
expected decrease in BP with pharmacologic vasodilators is 20
mmHG, but more profound decreases (over 50 mmHg) can occur [86].
- Sinus node dysfunction or 2nd or 3rd degree AV block: These
patients are at an increased risk of sinus arrest or prolonged
ventricular pauses and should not receive dypyridamole unless a
permenant pacemaker is in place [86].
- Xanthines (caffeine or theophylline/aminophylline) within the preceding 12 hours. Dipyridamole induced hyperemia is attenuated by caffeine [34,36]. A serum caffeine level of 2 mg/L or higher has been predicted to increase the likelihood for a false-negative exam [25]. The plasma caffeine half-life for healthy subjects is between 4.9 to 5.7 hours and most patients will have a caffeine level of less than 1 mg/L after a 24 hour abstinence [34]. However, the half-life of caffeine is prolonged in patients with underlying liver disease and in patients taking oral contraceptives, cimetidine, or rifampin [36]. A recent study indicated that approximately 19% of subjects who indicated no caffeine consumption within the previous 24 hours, had quantifiable serum caffeine levels [74]. Medications containing dipyridamole or verapamil should be discontinued 48 hours prior to the test [48].
- Carbamazepine treatment: Carbamazepine is used to control certain types of seizures. It is also used to treat trigeminal neuralgia. The agent can enhance the effects of adenosine A2A receptors and potentially cause profound heart block [86].
There is no contraindication to dobutamine in patients with renal dysfunction [127].
Side effects
Common, benign effects:
Side effects are common (50-60% of patients), but generally
benign and typically relate to the agents peripheral
vasodilatory effect. Chest pain (20-30%), flushing (15-30%),
lightheadedness (20%), headache (12-15%), nausea (5-10%),
extrasystoles (5%), mild hypotension (5%), and vomitting (rare).
ECG abnormalities characterized by ischemic ST-segment
depression (5%) is quite specific for the presence of CAD [8].
Chest pain is commonly atypical and is not an indicator of
coronary artery disease as it is observed in normal subjects as
well. The incidence of AV block is much less than that seen with
adenosine. Patients with baseline conduction abnormalities are
at greater risk for development of AV block (3.1% vs 0.3% for
patients without conduction abnormalities at baseline) [135].
Conduction abnormalities typically occur 2-3 minutes after
completion of the dipyridamole infusion and typically resolve
spontaneously or after administration of aminophylline [135].
Potentially more serious side effects include: (All are UNCOMMON)
1- Bronchospasm (0.2%)
Patients with a history of reactive airway disease or severe COPD may be at an increased risk for adenosine induced bronchospasm.
2- Severe cardiac ischemia and myocardial infarction (0.1%)
Dipyridamole does not increase myocardial oxygen demands as does dobutamine. Ischemia is likely due to a combination of factors including loss of coronary autoregulation, reduced coronary perfusion pressure in the presence of full coronary dilatation, and the "Coronary Steal" phenomenon (blood is preferentially shunted to non-stenotic vessels with a reversal of flow from the abnormal to normal vascular beds through collateral vessels).
3- Severe hypotension (BP systolic<100 mm Hg)
4- Ventricular dysrhythmia
Rare- when seen, it should raise the suspicion of underlying CAD [2].
5- Stroke
Most likely related to an intracerebral steal phenomenon in a patient with unilateral high grade ICA stenosis or generalized decrease in cerebral blood flow with a watershed phenomenon [9,10].
Treatment of side effects
The antidote for dipyridamole is Aminophylline which rapidly (within minutes) reverses its effects. Aminophylline is given by a slow I.V. infusion 1-2 mg/kg slowly (Typically 75-100mg is adequate, up to 250mg if necessary). Aminophylline competitively blocks endothelial adenosine receptors [8]. It DOES NOT reduce circulating adenosine levels which remain elevated as long as dipyridamole is present. (NOTE: The half-life of dipyridamole is longer than that of aminophylline and side effects may recur after aminophylline has been metabolized). Concominant administration of nitroglycerin is often helpful in reducing ischemia
Sensitivity/Specificity for the Dipyridamole Exam (SPECT pharmacologic imaging)
Sensitivity and specificity for dipyridamole stress myocardial perfusion are virtually identical to exercise testing: Sensitivity: 85-90%; Specificity: 80-90%. As with exercise testing, increased lung uptake of the tracer on dipyridamole imaging also correlates with the presence of coronary artery disease [8].
Other authors have found that thallium scintigraphy with pharmacologic stress had a lower diagnostic accuracy (80%) in characterizing the extent and distribution of CAD in patients without prior myocardial infarction [11].
Note that patients with type II diabetes may have a significantly decreased hyperemic flow response (and lower flow reserve) to dipyridamole that is likely multifactoral and related to microvascular disease, endothelial dysfunction, and abnormalities in regional sympathetic innervation [47]. Similarly, patients with end-stage renal disease may also demonstrate a suboptimal response to dipyridamole or adenosine stress [65].
Blunted heart rate: A blunted heart rate response to dipyridamole (max HR/rest HR < 1.2) has been linked to an increased risk of cardiac death, even in the presence of normal perfusion exam findings- for reasons not yet elucidated [56,70]. Patients with diabetes and chronic renal failure are more likely to have a blunted heart rate response to dipyridamole [56,68]. Patients on beta-blockers may still demonstrate a blunted heart rate response and this carries the same negative prognostic implications [70].
Treatment with beta-blockers has been show to decrease the coronary hyperemic response to dipyridamole (as measured by 13N-ammonia PET) and reduce the magnitude of inducible perfusion abnormalities on dipyridamole MPI [67].
Adenosine
Physiology & Pharmacology
Similar to dipyridamole, adenosine imaging reveals coronary flow reserve- there is a decreased hyperemic response in myocardial regions supplied by stenotic vessels. Flow reserve (an indicator of adequate collateral circulation) is a better predictor of subsequent cardiac events, as compared to percent stenosis as seen on angiography. A ratio greater than 2:1 between the flow in the normal and abnormal arteries is all that is necessary for detecting perfusion defects on pharmacologic stress perfusion scintigraphy. Antianginal medications have no impact on vasodilator pharmacologic stress since they do not interfere with vasodilator induced coronary hyperemia. Exogenous adenosine has a very short half-life (2-10 sec.) and therefore it requires a continuous infusion. The agent produces a mild dose related decrease in systolic and diastolic blood pressure, and a slight increase in heart rate.
Adenosine is a ligand of four distinct cell membrane receptors- A1, A2A, A2B, and A3 [49]. Adenosine produces coronary vasodilatation via activation of purine A2A receptors in a dose dependent manner and it produces more consistent and greater coronary vasodilatation than dipyridamole [34]. A2B receptors are also involved with vasodilatation [49]. A drawback of adenosine (and dipyridamole) is that these agents also non-selectively activate other adenosine receptors (A1 and A3) which are associated with undesirable side effects (such as dyspnea, flushing, chest pain, and A-V block) [41,49]. The A1 receptor mediates the negative inotropic, chronotropic, and dromotropic responses and can lead to the development of AV block [66]. It is believed that bronchoconstriction is due to mast cell activation/degranulation and immunoglobulin E and histamine release that are mediated by A3 receptors [58,118,137].
There is an underlying physiologic basis for why adenosine is so effective in producing coronary artery dilatation. In the setting of myocardial ischemia there is an immediate breakdown of adenosine triphosphate which generates increased circulating levels of adenosine. Adenosine acts to: 1) Produce vasodilatation in an effort to restore flow (dilates coronary arterioles by interacting with A2A receptors in the outer part of the endothelium and smooth muscle cell membranes) and 2) reduce A-V node transmission to protect the heart from sympathetic overstimulation.
Technique
Patient preparation is similar to that for dipyridamole.
Adenosine produces consistent vasodilatation in most patients at an infusion rate of 140ug/kg/minute for a 4 minute infusion [48]. The shorter infusion appears to be associated with less frequent side-effects, but the extent of the perfusion defect may be smaller than that seen with 6 minute infusions [30]. Maximal vasodilatation is generally observed within 2 minutes of initiation of the infusion. The infusion rate may be reduced to 75-100ug/kg if the patient experiences severe side effects and the response is almost instantaneous. The radiotracer injection is given midway through the infusion (2 minutes for a 4 minute infusion; 3 minutes for a 6 minute infusion). In high risk patients (recent MI, recent unstable angina, borderline hypotension, history of bronchospasm, or CHF), a step-wise increase in infusion rate may be performed. The infusion should begin at 50ug/kg/min. and increase to 75, 100, and 140 ug/kg/min at one minute intervals followed by injection of the tracer one minute after the highest infusion rate. The tracer should always be injected in a separate vein in the other arm to avoid giving a bolus of adenosine when the agent is flushed. Adenosine results in a modest increase in HR of 14 +/- 30 bpm [127]. Adenosine results in a modest decrease in systolic and diastolic BP (systolic decreases by 10 +/- 37 mmHg; diastolic decreases 8 +/- 19 mmHg) [127]. Early termination of the infusion should be considered for patients that develop severe hypotension (BP systolic less than 90 mm Hg), wheezing, chest pain associated with ECG evidence of ischemia (ST depression over 2 mm), and in patients that develop persistent second degree or complete heart block. Aminophylline is usually not necessary to reverse the adenosine due to the extremely short half-life of adenosine (2-10 sec.). ECG and hemodynamic monitoring is generally continued for 8 minutes after termination of the adenosine infusion [48].
Low level exercise can be combined with the adenosine infusion [62]. Slow walking on a treadmill during the adenosine infusion can: 1- help to decrease splanchnic activity (which may be problematic particularly with the technetium perfusion agents); 2- improve target-to-background ratio by increasing relative blood flow to the heart with exercise; 3- reduce the incidence of minor side effects (including AV block, sinus bradycardia, and hypotension [61]) by inducing a sympathetic response with exercise that offsets the hypotensive effects of adenosine; and 4- may result in greater ischemia detection than with adenosine alone [19,30,31,48,61,62]. Walking is usually done on a 0% grade at 1 mph simultaneous with the adenosine infusion [48]. Walking should not be performed for patients with left bundle branch block or ventricular pacing [48]. A delayed HR recovery after adenosine stress with low level exercise (≤ 12 bpm lower than peak HR) 5 minutes after adenosine infusion is predictive of an increased 5-year mortality [61].
Contraindications
Absolute Contraindications [127]:
- History of severe bronchospasm, active bronchospasm, and
moderate or severe COPD (moderate COPD is COPD with a
significant reversible component- FEV1 30-39% of predicted
with bronchodilator response >15% or FEV1 40-100% predicted
with a bronchodilator response >30%; and severe COPD is
FEV1 <30% predicted) [86].
- Sinus node dysfunction (sick sinus syndrome or symptomatic
bradycardia) or second/third degree AV block (unless pacemaker
is present).
- Wheezing or a history of severe bronchospasm or asthma: The bronchoconstricting effects of adenosine appear to be concentration dependent and more likely to occur at higher infusion rates (greater than 100 ?g/kg/min) [50]. Patients with stable mild asthma or COPD pre-treated with an inhaled beta-2-agonist may be able to tolerate adenosine stress when the infusion is titrated up to 140 ?g/kg/min over a 6 minute infusion [50]. Patients with mild asthma or COPD should not be currently on corticosteroid therapy, have no wheezing on auscultation at the time of testing, and no admission for an exacerbation during the past year [50]. None-the-less, use of a short-acting bronchodilator does not completely eliminate the risk of symptomatic bronchospasm [58] and up to 7% of mild asthma/COPD patients may develop intolerable symptoms necessitating discontinuation of the adenosine infusion and intervention [50]. In general, the bronchospasm resolves within a few minutes of termination of the infusion and administration of inhaled salbutamol [50]. Late bronchoconstriction after discontinuation of the adenosine infusion is unlikely [50].
- Hypotension (systolic BP less than 90-100 mmHg): The average
expected decrease in BP with pharmacologic vasodilators is 20
mmHg, but more profound decreases (over 50 mmHg) can occur [86].
The risk of serious hypotension may be higher in patients with
autonomic dysfunction, hypovolemia, left main coronary stenosis,
stenotic valvular heart disease, pericarditis or pericardial
effusions [127].
- Uncontrolled hypertension (systolic BP > 200 mmHg, or
diastolic BP > 110 mmHg [127].
- Use of xanthines (caffeine, aminophyllin, theophyllin) or
dipyridamole within the preceding 12 hours. Xanthines are
nonselective competitive inhibitors of adenosine receptors-
including A2A receptors [46,74]. These agents bind to the
receptor, but do not produce vasodilatory effects thereby
blunting the effect of adenosine resulting in a false-negative
exam [46].
Recent use of dipyridamole or dipyridamole containing medications (such as Aggrenox) [127]. Dipyridamole blocks adenosine transport into cells and may lead to very high blood levels and increased risk of serious side effects (such as profound heart block [86]). Medications containing dipyridamole or verapamil should be discontinued for 48 hours prior to the test [48,127].
It is widely held that adenosine induced hyperemia is
attenuated by caffeine [34]. The plasma caffeine half-life for
healthy subjects is between 4.9 to 5.7 hours and most patients
will have a caffeine level of less than 1 mg/L after a 24 hour
abstinence [34]. Some authors suggest that although the
adenosine induced heart rate response may be blunted by
caffeine, it does not affect adenosine-induced coronary
flow-heterogeneity and that abstinence from caffeine prior to
adenosine stress should not be a requirement [91]. This position
has yet to be supported by published guidelines [91].
- Known hypersensitivity to adenosine [127].
- Unstable angina, acute coronary syndromes, or less than 2-4
days after an acute MI [127].
- Carbamazepine treatment: Carbamazepine is used to control certain types of seizures. It is also used to treat trigeminal neuralgia. The agent can enhance the effects of adenosine A2A receptors and potentially cause profound heart block [86].
- Post-cardiac transplant: A higher incidence of 2nd and
3rd degree AV block has been described in cardiac transplant
patients receiving adenosine stress (up to 15% of patients), but
these effects are generally self limited and do not generally
require additional therapy [86].
Relative contraindications [127]:
- Profound sinus bradycardia (heart rate < 40 bpm)
- Mobitz type I second degree AV block (Wenskebach)
- Ingestion of caffeinated foods or beverages within the 12 hours prior to the exam
- Severe aortic stenosis (patients with severe AS are more likely to have a hemodynamically significant decrease in systolic BP with all vasodilator stress agents, but this is not typically associated with negative clinical events [141].
- Seizure disorder
There is no contraindication to adenosine in patients with renal dysfunction [127].
Side Effects
Side effects are very common and occur in about 80% of patients
[137]. Side effects also tend to be more intense than with
dipyridamole. Severe adverse effects that require discontinuation
of the infusion occur in 5% to 7% of patients. A complete lack of
even mild side effects (such as flushing) may raise the
possibility of unreported caffeine intake or of faulty adenosine
administration [48]. Aminophylline may be administered IV (50-250
mg) for reversal of severe side effects including severe
hypotension (BP systolic < 80 mmHg), symptomatic persistent
second degree or complete heart block, other significant cardiac
arrhythmia, wheezing, severe chest pain with ST depression of 2 mm
or greater, or signs of poor perfusion (pallor, cyanosis, cold
skin) [127].
Common, benign effects
Minor side effects are common and occur in approximately 80% of patients [127]. Common side effects include decreased blood pressure, increased heart rate, chest pain (25-30%), headache (11-35%), flushing (35-40%), SOB/dyspnea (20-35%- due to adenosine induced hyperventilation through stimulation of the carotid chemoreceptors and does not necessarily indicate bronchospasm), and GI discomfort (14%) [127,137]. Chest pain is usually atypical and does not correlate with the presence of CAD [127]. Ischemic ECG changes (ST depression) are seen in about 12% of patients and there presence is strong indicator of coronary artery stenosis. Heart rate increase appears to be lower in patients older than 70 years, males, diabetes, renal insufficiency, and in those with LV dysfunction (EF<40%) [61,123]. A blunted peak HR response to adenosine administration is associated with increased risk for cardiac death, independent of other variables [61,123].
More serious side effects include:
1- Cardiac bradyarrhythmias and heart block
Adenosine slows conduction in the proximal parts of the AV
node by stimulating A1 receptors and it also directly inhibits
the sinus node conduction. 1st degree A-V block (10%), 2d
(3.6%) or 3d degree block (very rare<1%) have all been
described. Episodes typically begin within the first 2 minutes
of the infusion and generally are very
transient/self-limiting, lasting only a few beats. If
prolonged, it will typically will resolve in 1 to 2 minutes
following discontinuance of the infusion. These effects may
also be prevented or ameliorated by having patients perform
even modest exercise to reduce vagal tone and increase
adrenergic stimulation of the conduction system [118].
Patients over 70 years of age have a higher risk of developing
AV block [136].
The incidence of AV block is much higher in orthotopic heart transplant patients (15-44%) and some authors suggest that adenosine should be avoided in these patients [80]. Regadenoson is associated with a significantly lower likelihood for AV block or bradycardia in heart transplant patients and may be a better agent for this patient population [80]. Adenosine should also be used with caution in patients following orthotopic liver transplant due to an increased risk of sinus arrest [43].
2- Bronchospasm
Infusion should be discontinued. Rarely intravenous
aminophylline infusion (50-100 mg) is required [48].
3- Myocardial ischemia
ST-segment depression of 1 mm or greater occurs in 5-7% of
cases [127]. In the presence of severe coronary stenosis with
well-developed collaterals, vasodilator administration can
decrease perfusion pressure supplying the collateral vessels
which can lead to ischemia [118]. Compared to chest pain, ST
changes may be indicative of true ischemia [127].
4- MI (extremely rare, but has been reported) [127].
5- New onset or recurrence of convulsive seizures may
infrequently occur [127].
Sensitivity & Specificity of the Adenosine Exam:
A sensitivity of 85-92% and a specificity of 90-95% have been reported for SPECT adenosine imaging. The incidence of cardiac mortality in patients with a normal adenosine stress test is low (1.3-2.3% per year), however, it remains higher than the incidence in patients with normal exercise MPS [72]. Myocardial stunning with decreased LVEF and wall abnormalities can be seen on gated images following both adenosine and dipyridamole stress and is an indicator of severe CAD [37,44].
ECG changes: The occurence of ST-segment depression during
vasodilator stress testing can be seen in 3-27% of cases [83].
Most patients with ST segment depression during vasodilator MPI
have reversible defects, and uncommonly (<10%) have normal
images [123]. The prognostic implications of ST-segment changes
vary depending on the presence or absence of perfusion defects
[123]. Adenosine induced ischemic changes on ECG convey a worse
prognosis (six-fold increase risk for cardiac events [123]) when
associated with reversible perfusion defects on MPS (SSS greater
than or equal to 4) and the finding is associated with left-main
disease and extensive CAD [72,83,123]. However, if the MPS is
normal, there are conflicting reports [72,83]. For patients with
normal perfusion scans, some studies suggest that this discordant
pattern is associated with an increased likelihood for
multi-vessel CAD and a increased risk for adverse cardiac events,
while others suggest the association with obstructive CAD is poor
(as long as the patient does not have multiple coronary risk
factors- particularly diabetes, and no history of prior MI or
CABG) [72,82,83,123]. Proposed explanations include microvascular
disease and the presence of collateralized occluded vessels [123].
ST-segment depression with pharmacologic stress also seems to be
more common in women than in men (in studies, 77-92% of patients
with this finding are women) [82,123].
Blunted heart rate response: As with dipyridamole and
regadenoson, a blunted heart rate response to adenosine has been
described as an independent predictor of a poor outcome/associated
with an adverse prognosis [68,81,97]. The blunted heart rate
response to adenosine is likely related to autonomic cardiac
dysfunction/cardiac autonomic neuropathy [81,97]. A blunted heart
rate response to pharmacologic stress is associated with older
age, diabetes, metabolic syndrome, chronic kidney disease, and
beta blocker use [81,107]. Studies have demonstrated a graded
relationship between blunted heart rate response and risk for
cardiac mortality (HRR 15 (0.8%) [107]. Importantly, patients with abnormal
perfusion and reduced heart rate response have the highest risk
for cardiac events [107].
Beta-blockers prevent an increase in myocardial oxygen demand and
attenuate exercise induced ischemia [67]. Beta blocker withdrawal
has been shown to result in an increase in adenosine MBF compared
to not discontinuing the medication (about an 8% increase in MBF)
[111]. However, studies have suggested that beta-blocker therapy
does not seem to diminish the ability of the pharmacologic
adenosine exam to detect clinically significant CAD, and, more
importantly, patients with normal exams on beta-blockers still
have a low mortality risk [63,111]. Although more recent study
does suggest that beat-blockers can reduce the diagnostic
sensitivity of the adenosine exam, by reducing the ability of
adenosine to provoke myocardial blood flow heterogeneity [67].
This may be multifactoral and related to suppression of
adrenergically mediated changes in vasomotor tone of the coronary
arteries and enhanced subendocardial perfusion by prolonging
diastole (due to lower heart rates) and reducing wall stress
[67,111]. Beta blockade may also result in a significant reduction
in adenosine-related side effects- especially chest pain [67].
However, discontinuing beta-blockers for MPI can place patients at
increased risk for angina and acute ischemic events and this needs
to be considered before stopping the agents [67].
Clopidogrel (Plavix) is antiplatelet agent used for the
prevention of stent thrombosis after coronary and epripheral
vascular stenting [128]. The agent acts via an adenosine
diphosphate receptor which is present on the platelet membrane
(inhibiting platelet activation and aggregation), but also found
on the membrane of vascular wall cells [128]. The agent has been
shown to modulate vasorelaxation and to improve microvascular
endothelial function independent of its platelet inhibitor effects
[128]. The agent has not been shown to affect adenosine or
exercise stress test results [128].
Transient ischemic LV dilatation:
TID can be observed in patients that undergo adenosine stress
[93]. For a dual isotope exam, a TID > 1.36 has a sensitivity
of 71%, and a specificity of 86%, for severe and extensive CAD
[93]. For a same day sestamibi rest-stress protocol, a TID ratio
of over 1.31 has been shown to represent the top quartile
[94].
A2A receptor agonists: Regadenoson
There are multiple adenosine receptor subtypes (A1, A2A,
A2B, and A3) which are all non-selectively
activated by adenosine [92]. The A2A receptor
stimulated coronary vasodilatation, but the other receptors have
undersireable side effects (A1 - atrioventricular
block; A2B - peripheral vasodilatation; and A2B
and A3 - bronchoconstriction) [92]. Newer pharmacologic
agents have been developed (such as binodenoson and regadenoson)
which will more selectively target the A2A receptor
with the hope that these will produce fewer unwanted side effects
(A2A receptors are loclized on the surface of coronary
arterial smooth muscule cells [78]) [41,49,58].
Regadenoson's affinity for A2A receptors is 9 fold
greater than its affinity for A1 receptors, and it's
affinity for A2B, and A3 is minimal [58].
Compared to adenosine, regadenoson is 100 times more potent at the
A2A receptor [85].Transient QTc prolongation has been
reported after regadenoson though without clinical significance
[85]. Despite a lower plasma concentration in obese patients, BMI
does not appear to alter the efficacy of regadenoson [79].
Regadenoson has a triphasic half-life [78,86]. Regadenoson
reaches a maximal plasma concentration within 1-4 minutes after
injection [64]. The agent promotes peak hyperemia (greater than
85% of peak maximal flow) within 30 seconds of the bolus injection
(range 20-40 seconds) [75,100]. The injection induces an initial
phase of a 2-3 fold increase in myocardial blood flow with an
initial half-life of 2-4 minutes (mean duration of action of 2.3
minutes [75]) [64,66,78,100]. Although other authors suggest that
the mean duration of increased flow (two fold or greater) is 8.5
minutes [119]. A second phase then ensues, with a half-life on
average of 30 minutes with a gradual loss of the pharmacodynamic
effect [64]. The final phase consists of a decline in plasma
concentration with a half-life of approximately 2 hours [64,87].
The agent has a terminal half-life of 33-108 minutes [78]. If the
agent needs to be re-administered, an interval of 2.5 hours is
recommended prior to redosing [132]. Aminophylline can be used to
treat side effects, however, aminophylline will block the peak
blood flow response and hemodynamic effects of regadenoson
[85,86]. The current recommendation is to avoid
caffeine-containing products for at least 12 hours prior to
regadenoson administration [66]. In an animal model, the presence
of metoprolol has been shown to decrease the duration of the
regadenoson-induced increase in myocardial blood flow, but not the
peak flow and the duration was still adequate for diagnostic
purposes [84].
The primary hemodynamic effects regadenoson are an increased
heart rate (mean max increased of about 21 bpm) and a decrease in
blood pressure (SBP decrease of 24 mm Hg, DBP decrease 12 mm Hg)
[66]. Two mechanisms appear to account for the tachycardia induced
by regadenoson. First, peripheral vasodilatation leads to a fall
in BP, triggering a baroreflex-mediated activation of the systemic
nervous system and a subsequent increase in HR [87]. Second,
evidence from animal models suggests that regadenoson also causes
a direct sympathoexcitation through stimualtion of arterial
chemoreceptors in the carotid bodies via A2A receptors
with increase in plasma norepinephrine [87,132]. This presumably
causes the brief mini-panic attack feeling that patients often
experience beginning 30-90 seconds after administration of
regadenoson or adenosine [132]. The maximal BP changes occur
within 5 minutes of infusion and return to near baseline within 15
minutes [85]. In summary, regadenoson induces a more intense
increase in heart rate than adenosine and a comparable decease in
BP [81,85,102]. However, other authors indicate that the response
of systolic BP to regadenoson is variable- increasing in some and
decreasing in others [95]. The hypotensive response is likely
related to A2a receptor activation, while the hypertensive
response is likely elicited by stimulation of A2A recptors in the
carotid body (that results in norepinephrine release) [95].
Despite the greater increase in HR compared to adenosine,
regadenoson does not seem to produce septal perfusion defects in
patients with LBBB or cardiac pacers [106].
Blunted heart rate response:
A blunted heart rate response to pharmacologic stress is a marker
of autonomic dysfunction [124]. A blunted HR response to
regadenoson has been described in patients with diabetes,
metabolic syndrome, insulin use, patients with decreased LVEF,
patients with end-stage renal disease, older patients, and
aldosterone antagonist use [75,78,81,133]. In diabetics and
patients with metabolic syndrome this blunted response may be
related to an impaired sympatho-excitation secondary to
chronotropic incompetence (ie: cardiac autonomic neuropathy)
[75,78]. The blunted HR response is dissociated from the BP
response and carries adverse prognostic value on top of
traditional MPI findings with decreasing heart rate response
associated with a step-wise increase in mortality [78,81,104]. In
one study, there was a stepwise association between decreasing HR
and increasing risk of death, with a less than 17% increase in HR
associated with the greatest risk for all cause mortality
[81]. In another study, a blunted heart rate response was
associated with a 2.75 fold increase in the risk of death, a 70%
increase in the risk of cardiac death or MI, and an 83% increase
in the risk of cardiac death, MI, or late coronary
revascularization [140]. Proposed guidelines suggest that a HRR
< 15% should be considered blunted, > 30% normal, and 15-30%
as intermediate [126].
For patients with end-stage renal disease, a blunted heart rate
response (<28%) provides incremental prognostic information
(regardless of the perfusion exam findings) and is associated with
an increased risk of cardiovascular events and death (adjusted
hazards ratio 2.75) [124,125].
The use of a beta-blocker during the exam does, however, decrease
the normal increase in HR from regodenoson [84,85]. IV
aminophylline (25-100mg) is effective in abbreviating the coronary
vasodilatory effect of regadenoson, but not the heart rate
response [66]. An artificially blunted heart rate response can be
observed in patients with RV pacers [106].
Regadenoson induced ECG changes: ST segment depression
following regadenoson is associated with an increased prevalence
of severe coronary artery disease and higher rates of major
adverse cardiac events, independent of MPI findings and clinical
co-morbidity [114]. Some authors suggest that for regadenoson
stress an ST depression of 0.5 mm or more is associated with an
higher risk for severe CAD and major adverse acrdiac event,
irrespective of the MPI findings [115]. Use of 1.0 mm ST
depression results in improved specificity, but decreased
sensitivity [115].
Technique:
Regadenoson is given as a fixed dose bolus injection of 400 mcg
(0.4 mg) given over 10 seconds with a 5 cc saline flush [66].
Radiotracer is injected 10-20 seconds later [66,85]. Some authors
suggest the routine use of 75mg of aminophylline two minutes after
regadenoson injection or 90 seconds after radioisotope injection
to aid in reducing the freqency and severity of adverse effects of
regadenoson (particularly GI side-effects) [90].
Combining low-level exercise with regadenoson infusion has been shown to be feasible and is well tolerated with overall improved image quality (due to decreased gut and liver activity) and decreased frequency of side effects [62,66,71,85]. Some authors feel that it is unlikely that mild exercise (stage I of a Bruce or modified Bruce protocol) will provide enough hemodynamic or ECG data to be clinically relevant or that it will profoundly reduce sub-diaphragmatic interference with cardiac activity [105].
Because Regadenoson is supplied as a read to use syringe for
bolus administration (unlike adenosine which requires an infusion
pump and dose adjustment) the agent can be quickly administered in
cases in which patient's fail to obtain adequate exercise stress
[101]. Some authors suggest that Regadenoson can be given safely
following submaximal exercise stress testing in order to obtain
diagnostic perfusion exams with better target to background ratios
and less frequent interference from sub-diaphragmatic activity
[96,101,102,138]. Some patients can experience a significant rise
or drop in blood pressure if the agent is administered at the peak
of symptom-limited exercise and there is a greater safety margin
if the agent is given during the walk recovery period [104]. In
patients with submaximal exercise, they should transition to a
slow walk recovery (treadmill speed gradually reduced from 1.7 to
1.2 mph at 0% grade) for 3 minutes prior to regadenoson
administration and they should continue walking for another 2
minutes at 1.2 mph and 0% grade following regadenoson
administration [143]. Although chest pain and dyspnea are more
frequently observed with the use of Regadenoson following
submaximal exercise, other common side effects such as flushing,
dizziness, lightheadedness, or GI upset are seen less frequently
[96]. However, the manufacturers package insert also warns that an
excessive hypertensive response can be seen following regadenoson
administration- particularly in patients with underlying
hypertension or undergoing combined low-level exercise [104].
Finally, regadenoson should NOT be given to patients following
submaximal exercise if they developed symptoms or ECG evidence of
ischemia during exercise stress or during the recovery phase
[138,143]. If a patient undergoing exercise stress develops chest
pain and ischemia ECG changes, they have achieved an ischemic
endpoint, regardless if the heart rate is < 85% of maximum
predicted [143]. In patients with equivocal symptoms or equivocal
ECG changes, it would also be prudent to exercise caution and not
administer regadenoson before one hour to allow the patient to
return to a baseline state [143].
Metabolism:
Regadenoson, unlike adenosine, is not metabolized and
predominantly excreted unchanged via tubular secretion by the
kidneys (55-60%), while the remaining 40% is excreted by the liver
(also unchanged) through the bile [75,85,87]. In patients with
renal impairment, renal clearance of the agent is decreased
resulting in prolonged elimination half-lives [64,78]. This is not
a problem with adenosine which is promptly cleared from the
circulation by cellular uptake, predominantly by erythrocytes and
vascular endothelial cells [64]. Once inside the cell, adenosine
is quickly metabolized either phosphorylation by adenosine kinase
to adenosine monophosphate, or via deamination by adenosine
deaminase in the cytosol to iminase [64]. Hence, adenosine
elimination is not affected by renal function [64]. However,
regadenoson appears to be safe to use in patients with chronic
kidney disease not on dialysis (GFR<60; even stage 3 and 4
chronic kidney disease [87]) with minimal additional side effects
and a favorable hemodynamic response [78,85,87,103]. Note- one
study reported a higher incidence of PVC's in ESRD patients
following regodenoson [103]. Other authors have also noted a
greater prevalence of headaches and GI symptoms such as diarrhea
and abdominal discomfort [134]. However, these side effects can be
substantially reduced by the prophylactic administration of 75 mg
of aminophylline (which inhibits A2a receptor activation) 90
seconds following radioisotope administration [134].
In patients with liver dysfunction, the agent appears to be well tolerated, although the HR response appears to be lower than in control subjects [75,105]. The presence of ascites in patients with liver disease can lead to overestimation of the patients true weight which results in larger doses of adenosine or dipyridamole with potentially more side effects [75]. Because regadenson is given as a fixed dose, this is not an issue [75].
Contraindications to Regadenoson:
- Sinus node dysfunction (sick sinus syndrome or severe
bradycardia) and high-degree second or third A-V block in the
absence of a functioning artificial pacemaker [118,127].
- Patients with bronchospasm that are actively wheezing at the
time of the stress test or have a history of significant reactive
airways disease should not receive regadenoson [118,127].
- Systolic BP below 90 mm Hg. Note- the risk of serious
hypotension may be higher in patients with autonomic dysfunction,
hypovolemia, left main coronary stenosis, stenotic valvular heart
disease, or pericarditis or pericardial effusion [127]
- Uncontrolled hypertension (systolic BP > 200 mm Hg, or
diastolic > 100 mm Hg) [127]
- Recent (< 48 hours) use of dipyridamole or dipyridamole
containing medications (Aggrenox) [127]
- Known hypersensitivity to adenosine or regadenoson
- Unstable angina, acute coronary syndrome, or less than 2-4 days
after an acute MI
Relative contraindications to Regadenoson [127]:
- Profound sinus bradycardia (HR < 40 bpm)
- Mobitz type I second degree AV block (Wenckebach)
- Severe aortic stenosis
- Ingestion of caffeinated food or bevergaes within the preceding
12 hours
- Seizure disorder (Regadenoson may lower the seizure threshold)
Side effects:
Adverse effects can be experienced by up to 66% of patients that
receive regadenoson, but are mostly mild in intensity [92,137].
Patients with asthma or COPD are at an increased risk of
adenosine induced bronchospasm via activation of the A2B,
and A3 receptors [85]. Even with regadenoson, between 18-61% of
COPD patients may experience dyspnea during the infusion (dyspnea
is seen in about 11% of patients with asthma [92]) [58,92]. The
dyspnea is generally described as mild (67%) and is severe in only
3% of patients [58]. Interestingly, the dyspnea does not appear to
be associated with true bronchospasm [58,59,92] or significant
oxygen desaturation [85]. However, other authors have reproted
bronchospasm following Regodenoson infusion [101] and caution is
advised if considering using regadenoson in patients with COPD or
asthma as severe reactions could potentially occur, but the agent
is not contraindicated [92,118]. Regadenoson is not FDA approved
in patients with ESRD, but it has been used off label in some
cardiology labs [117].
Other side effects include headache (1.4-29%), flushing (12-17%),
chest discomfort (11-13%), dizziness (7-19%), chest pain (7-35%),
and nausea (2-12%) [66,71,127]. Most adverse reactions begin soon
after dosing (and within 2 hours) and generally resolve within
approximately 15 minutes, except for headache which generally
resolves in 30 minutes [92127].
Aminophylline (dose 50 to 250 mg via slow IV infusion over 30 to 60 seconds) can be given to attenuate severe or persistent adverse reactions [127]. If aminophylline is not available, IV caffeine citrate 65 mg diluted in 25 cc D5W can be infused over 3-5 minutes with similar effective results [139]. Oral caffeinated beverages such as coffee or diet colas have also been shown to be effective at reversing side effects [139]. The routine administration of 75 mg of aminophylline to all patients following the uptake phase of the exam substantially decreases mild side effects (approximately 5 minutes following tracer administration)[118,139]. Routine aminophylline administration can decrease the incidence of GI symptoms by 50%, headache by 70%, and any related adverse effect by 34% [142]. Some suggest that aminophylline can be administered as early as 90-120 seconds following radioisotope injection [142], but premature administration of the agent could potentially blunt a stress-induced perfusion abnormality [142]. Patients with severe chronic kidney disease experience more frequent GI adverse effects from regadenoson, but aminophylline administration following regadenoson reduces the incidence of these adverse effects [117].
Rhythm or conduction abnormalities can be seen in up to 26% of
patients [127]. Transient QTc prolongation can occur [88,92].
First degree AV block can be seen in 3% of patients and
second-degree block in 0.1% [127], in contrast to Adenosine in
which the incidence of 2nd or 3rd degree heart block is 4-5% [71].
However, heart block (including third degree) and asystole have
occured with the agent (and the risk for asystole may be increased
in patients receiving n-acetylcysteine treatment) [77,88,99,144].
QT interval prolongation has also been reported and extra care
should be taken if the agent is given to patients with baseline QT
interval prolongation or in patients taking concomitant drugs with
the potential for QT prolongation [98]. Angina pectoris or ST
depression can be seen in 12% of patients [66]. Hypersensitivity
reactions including angioedema, uticaria, and anaphylaxis have
been described [88], as has coronary vasospasm [129].
Additonal online side effects have been reported by Astellas
Phamaceuticals (http://www.lexiscan.com/home.aspx):
| IMPORTANT SAFETY INFORMATION |
| Do not administer Lexiscan to patients with second- or third-degree AV block or sinus node dysfunction unless these patients have a functioning artificial pacemaker. |
| Fatal cardiac arrest, life-threatening ventricular arrhythmias, and myocardial infarction may result from the ischemia induced by pharmacologic stress agents. Hypersensitivity including anaphylaxis, angioedema, cardiac or respiratory arrest, respiratory distress, decreased oxygen saturation, hypotension, throat tightness, urticaria and rashes have occurred. Resuscitation equipment and trained staff should be immediately available before administering Lexiscan. |
| Adenosine receptor agonists, including Lexiscan, can depress the SA and AV nodes and may cause first-, second-, or third-degree AV block, or sinus bradycardia requiring intervention. In postmarketing experience, heart block (including third degree), and asystole within minutes of Lexiscan administration have occurred. |
| Adenosine receptor agonists, including Lexiscan, induce arterial vasodilation and hypotension. The risk of serious hypotension may be higher in patients with autonomic dysfunction, hypovolemia, left main coronary artery stenosis, stenotic valvular heart disease, pericarditis or pericardial effusions, or stenotic carotid artery disease with cerebrovascular insufficiency. In postmarketing experience, transient ischemic attack, seizures and syncope have been observed. |
| Adenosine receptor agonists, including Lexiscan, may result in clinically significant increases in blood pressure in some patients. In postmarketing experience, cases of potentially clinically significant hypertension have been reported, particularly in patients with underlying hypertension and when low-level exercise was included in the MPI. |
| Adenosine receptor agonists, including Lexiscan, may cause dyspnea, bronchoconstriction and respiratory compromise. Appropriate bronchodilator therapy and resuscitative measures should be available prior to Lexiscan administration. |
| The most common adverse reactions (≥5%) to Lexiscan are dyspnea, headache, flushing, chest discomfort, angina pectoris or ST-segment depression, dizziness, chest pain, nausea, abdominal discomfort, dysgeusia, and feeling hot. Most adverse reactions began soon after dosing, and generally resolved within approximately 15 minutes, except for headache, which resolved in most patients within 30 minutes. Aminophylline was used as a reversal agent in 3% of patients. |
| In postmarketing experience, QTc prolongation, tremor, abdominal pain in association with nausea, vomiting, or myalgias, and diarrhea, fecal incontinence, wheezing and musculoskeletal pain have occurred. |
Since it's release other potential complications such as asystole
leading to hemodynamic collapse, advanced heart block, transient
QTc prolongation, new onset atrial fibrillation with rapid
ventricular response, atrial flutter, seizures, and
cerebrovascular accidents have been reported [109,110,116].
Additionally, the FDA has also released a safety announcement
regarding a risk of heart attack or death- particularly in
patients with unstable angina or cardiovascular instability [108].
Finally, case reports of asystole have been reported [108] and the
use of atropine may be more effective at reversing this
hemodynamic effect than aminophylline [110].
Potential epileptogenic mechanism: Seizures can also occur-
particularly in patients with a history of seizure disorders (even
when stabilized), but seizure can also occur in patients with no
history of a seizure disorder [88]. The seizure typically occurs
wihtin 2-5 minutes of administration [88]. The seizure can quickly
evolve from partial to secondary generalized [88]. Aminophylline
has been shown to have no effect on decreasing seizure activity,
and can actually perpetuate the seizures by lowering the seizure
threshold [88,118]. If seizures occur, benzodiazepines should be
available to treat this potential side effect [88]. It has been
suggested that the seizures are related to stimulation of CNS A2A
receptors located in the striatum, nucleus accumbens, tuberculum
olfactorium, cortex, and hippocampus may play a role in initiation
of seizures [109].
Sensitivity/Specificity and Prognostic Value:
Major cardic events are infrequent in patients with normal
regadenoson MPI and provides similar prognostic data to a normal
adenosine MPI exam (a one year 1.1% incidence of cardiac death,
myocardial infarction, or coronary revascularization)
[104,113,118]. Cardiovascular risk increases according to the
extent and severity of the myocardial perfusion defect [119,120].
The agreement rates for adenosine and regadenoson SPECT imaging is
greater than 90% [85].
Regadenoson is generally better tolerated than adenosine [85].
Transient ischemic LV dilatation:
TID can also be observed with regadenoson imaging (up to 6% of
patient scans [131]) and is associated with the presence of
multi-vessel CAD [93]. For dual isotope imaging, a TID ration
above 1.39 has a specificity of 95% and a sensitivity of 15% for
determining multi-vessel CAD [93]. For single isotope Tc-99m agent
imaging, a TID ratio of 1.31-1.33 has been shown to be abnormal,
but the finding has poor discriminatory capacity in identifying
severe and extensive CAD [112] (the increased risk associated with
TID appears to be most apparent only in patients with abnormal MPI
perfusion findings [123,130]).
Dobutamine:
Indications:
1- Dobutamine can be used in patients that are unable to exercise and have contraindications to adenosine (severe reactive airway disease, high grade A-V block, arterial hypotension, or methylxanthine medication).
2- Dobutamine can also be used to assess contractile reserve:
Gated SPECT imaging can provide incremental information to perfusion images. Many conditions can lead to wall motion abnormalities, but some of the conditions are reversible. For instance, on SPECT imaging both subendocardial myocardial infarction and hibernating myocardium can produce a non-transmural perfusion defect [18]. Both conditions can also demonstrate associated wall motion abnormalities, however, hibernating myocardium will demonstrate improved contractility following revascularization. Following an acute MI, areas of stunned myocardium will also demonstrate wall motion abnormalities on gated exams, but will gradually return to normal function. Contractile reserve refers to an incremental improvement in wall motion with dobutamine stress.
A low dose infusion of dobutamine (5-10 ug/kg/min) during gated SPECT image acquisition can be performed and compared to a rest gated exam. SPECT imaging is usually started 3 minutes following initiation of the dobutamine infusion [24]. Hypokinetic segments that demonstrate improved contractility during the dobutamine infusion indicate a high likelihood for functional improvement following revascularization [24]. A global increase in LVEF of more than 5 is also a good predictor of post-revascularization functional improvement [16,17]. The low dose dobutamine SPECT examination has the added benefit of providing simultaneous perfusion information which cannot be assessed with dobutamine echocardiography [3].
Physiology & Pharmacology
Dobutamine is a synthetic sympathomimetic amine. It is a potent stimulator of beta-1 receptors and a mild beta-2 (increasing myocardial contractility, atrioventricular ocnduction, and positive chronotrophic effects), and alpha-1 agonist (produces systemic vasocontriction) [27,57]. The agent has more inotropic than chronotropic activity at low doses (4-8 ug/kg/min). At high doses used for pharmacologic stress (greater than 10 - 20 ug/kg/min.) it increases both inotropic and chronotropic action of the heart. The increase in myocardial contractility and heart rate result in increased oxygen demand and an increase in blood flow in normal coronary arteries [27]. Hence, the agent produces hemodynamic changes that mimic those produced by exercise. Dobutamine undergoes rapid metabolism in the liver, resulting in a short biological half-life of approximately 2 minutes [27], but its physiologioc effect may persist for 5-20 minutes [86]. Unlike dopamine the agent does not produce a significant peripheral vasoconstriction.
Myocardial oxygen demand is increased due to:
- Increased heart rate
- Increased myocardial contractility
- Increased systolic blood pressure
Thus, the agent actually provokes ischemia, but the increase in coronary blood flow is less than that observed with dipyridamole or adenosine. Generally, flow is increased between 2 to 3 times baseline. Some centers augment the infusion with atropine in order to get an even higher heart rate.
Arbutamine is an analog of dobutamine which has a much shorter half-life that is presently being evaluated for use in pharmacologic stress exams [20]. The agent is a mixed beta-1 and beta-2 agonist with a mild affinity for alpha-1 receptors and less peripheral vasodilating activity [21]. The agent is delivered via a closed loop computer system that constantly monitors the heart rate response [21]. Attenuation of MIBI uptake and diminished defect contrast are also observed with arbutamine stress [20].
Dobutamine in Tc-sestamibi imaging:
Uptake of Tc-sestamibi may be attenuated during dobutamine stress when compared to 201Tl uptake [20]. Defects on Tc-sestamibi perfusion exams are less pronounced than adenosine induced defects at the same flow heterogeneity between normal and stenotic zones [20]. Mild stenoses can be missed using Tc-sestamibi and dobutamine stress (such defects are better detected by using 201Tl) [20]. The reduction in defect magnitude is felt to be related to enhanced calcium influx with increased intracellular calcium during dobutamine infusion which results in altered sestamibi mitochondrial membrane binding [20]. Sestamibi uptake can be enhanced during dobutamine effusion by injecting ruthenium red which is a selective inhibitor of mitochondrial calcium influx [20].
Contraindications to dobutamine [127]:
- Recent myocardial infarction (less than 2-4 days)
- Unstable angina/acute coronary syndrome
- Uncontrolled heart failure
- History of ventricular tachycardia
- Atrial fibrillation or other atrial tachyarrhytmias with an uncontrolled ventricular response
- Uncontrolled hypertension (systolic BP . 200 mmHg or diastolic BP > 110 mm Hg) [30]
- Left ventricular outflow tract obstruction (hypertrophic
obstructive cardiomyopathy) [86]
- Severe aortic stenosis
- History of aortic dissection or aortic aneurysm
- Known hypersensitivity to dobutamine
- Left bundle branch block- similar to exercise stress, dobutamine stress may result in apparent septal perfusion defects and vasodilator stress should be used in these patients [27]
Relative contraindications for dobutamine [127]:
- Patients on beta-blockers where the heart rate and inotropic response to dobutamine will be attenuated
- Severe aortic stenosis
- Symptomatic or large aortic aneurysm
- Left bundle branch block
- Paced ventricular rhythm
There is no contraindication to dobutamine in patients with renal
dysfunction [127].
Technique
It is usually recommended that beta-blockers be withheld for at least 48 hours prior to the test because these agents will reduce the inotropic and chronotropic of dobutamine [27]. Calcium channel blockers and beta-blockers should be discontinued for 24 hours prior to the exam if possible, or at least not taken on the day of the study.
The agent is given intravenously by a graded infusion beginning at 10 ug/kg/min. and increased by 10 ug every 3 minutes to a maximum infusion of 40 ug/kg/min. The tracer is injected one minute after the final increase and the infusion is continued for an additional 1-2 minutes. Generally a heart rate target of 85% of predicted maximum is used [48]. If the patient reaches a satisfactory hemodynamic response in double product or develops untoward side effects, the injection of the radiotracer may be made sooner. The infusion should be terminated if the patient develops a ventricular tachycardia or ST segment elevation.
In the majority of patients, incremental doses of dobutamine
induce a progressive increase in heart rate [27]. Some patients
have a plateau of heart rate response- particularly those
receiving beta-blockers [27]. If the heart rate has not doubled
with dobutamine by the 7:30 minute mark, it is unlikely that the
patient will reach 85% of the target heart rate. Atropine can be
used to augment increasing the heart rate in patients that fail to
achieve 85% of maximal heart rate at peak infusion [27,86].
Atropine is a parasympatholytic agent that blocks the cardiac
action of the vagus nerve and it augments myocardial oxygen
consumption by increasing the heart rate. The onset of action
peaks in 2 to 3 minutes. Atropine 0.6 mg is injected intravenously
and can be administered in incremental doses up to a maximum of 2
mg [27]. However, a maximum atropine dose of less than 1 mg is
advisable in elderly patients and in those with small body
habitus, as these groups can be more prone to developing
neuropsychiatric syndromes as a side effect of atropine [76].
Atropine in contraindicated in patients with narrow angle glaucoma
[86].
Potential complications include sinus tachycardia or atrial tachyarrhythmia. A beta blocker such as metoprolol 5 mg intravenously reverses the effects of atropine and can also be used to reverse the effects of dobutamine [13]. Atropine is contraindicated in patients with narrow angle glaucoma, myasthenia gravis, obstructive uropathy, or obstructive gastrointestinal disorders [27].
Criteria for termination of the test are severe chest pain, ST-segment depression greater than 2 mm, ST-segment elevation in patients without previous myocardial infarction, significant ventricular or supraventricular arrhythmia, hypertension (BP greater than 240/120 mmHg), and systolic blood pressure drop of greater than 40 mm Hg [27].
Side Effects
With dobutamine side effects are frequent (up to 70-80% of
patients- dobutamine carries the highest risk for adverse events
of all the stress modalities) and are more common in the elderly
[27,118]. In fact, the dose rate must be lowered in about 25% of
patients due to the presence of side effects. Non-cardiac side
effects include nausea, headache (15%), flushing, chills, dyspnea,
and anxiety [27]. Common cardiovascular side effects include chest
pain (13-30% of patients and does not necessarily correlate with
the presence of ischemia [57]), palpatations (30%- atrial
fibrillation, short run supraventricular tachycardia), and angina.
Angina with ST segment depression occurs in 50% of patients with
coronary artery disease (other authors indicate ischemic ST
depression in one third of patients [127]). Premature ventricular
contractions are common, but sustained cardiac arrhythmias such as
paroxysmal atrial tachycardia and ventricular tachycardia are
uncommon. Patients at risk for arrhythmias are those with a
history of arrhythmias, hypokalemia, and left ventricular
dysfunction or extensive fixed perfusion defects [27].
Dobutamine-induced ventricular arrhythmias can be effectively
treated with IV beta blockers, such as esmolol, 0.5 mg/kg over 1
minute or IV metoprolol (5 mg) [118,127].
Systolic blood pressure may progressively increase, progressively decrease, or manifest a biphasic response (initial increase at a low dose followed by a decrease at high dose) [86]. Dobutamine-stress induced hypotension (a 20 mm Hg or greater decrease in blood pressure likely related to a beta-2 adrenergic agonism) occurs in about 15% of patients [27,30]. Other potential life-threatening adverse effects include myocardial infarction, LV wall rupture, and asystole [57].
Dobutamine is known to increase the risk of ventricular
tachyarrhythmias, especially at higher doses, because of
accelerated diastolic depolarizations.
The infusion should be terminated if the patient develops intolerable side effects such as chest pain, headache, tremors, palpatations, severe ischemia, or major arrhythmia [86]. Side effects that do not resolve after termination of the dobutamine infusion or severe hypertension (BP systolic > 200 mmHg, BP diastolic > 110 mm Hg), significant cardiac arrhythmia, or severe chest pain associated with ST depression of 2 mm of greater can be treated with a short acting I.V. beta-blocker such as metoprolol (1-5 mg) or esmolol (0.5 mg/kg over 1 minute) I.V. [27,127].
Atropine intoxication is a central anticholinergic syndrome causing confusion or sedation [27]. It can be treated by 0.5-2.0 mg physostigmine I.V. [27].
Sensitivity and specificity:
For the detection of coronary artery disease dobutamine stress testing has an overall sensitivity of 82-88% (95% confidence interval 83-90%), a specificity of 72-75% (95% CI 70-77%), and an accuracy of 83-84% (95% CI 80-87%) [21,27,30,33]. Sensitivity is higher in patients with multivessel disease (92-97%), than for patients with single vessel disease (80%) [27]. The exam can be inconclusive (failure to achieve target heart rate in the absence of perfusion abnormalities) in 9-10% of patients [26,27]. In a comparison between dobutamine stress imaging and dobutamine echocardiography the sensitivities were 86% and 80%, respectively; specificities were 73% and 86%, respectively; and the accuracies were 82% and 82% respectively, [27]. However, the overall sensitivity for the detection of coronary artery disease is lower than with adenosine stress which produces greater flow heterogeneity [45].
Dobutamine stress imaging has been shown to provide incremental prognostic information in the evaluation of patients with known or suspected coronary artery disease [26,27]. Patients with normal scans have an annual risk for cardiac events of 0.8% to 1.2% (cardiac death rate 0.9%), while patients with abnormal exams have an annual risk for cardiac events of 4.4% to 9.2% (cardiac death rate 2.7%) [26].
Dobutamine Tc-myoview imaging (either alone [39] or with atropine [23]) has been shown to provide incremental prognostic information to clinical and stress test data [23,39]. A normal exam is associated with a very low probability for cardiac events (cardiac death rate of 1% or less per year) [23,39]. The cardiac death rate increases to 4.3-5.1% in patients with abnormal scans [23,39]. These findings are similar to Tc-sestamibi results [23]. In general, the cardiac event rate tends to be relatively higher in patients with normal pharmacologic exams compared to those with normal exercise stress exams [23]. This is likely in part related to the higher risk status of patients referred for pharmacologic testing [23].
REFERENCES:
(1) Wong, Ann Intern Med 1992
(2) Nucl Med Annual 1994, p.129
(3) J Nucl Med 1994; Pennell DJ, Ell PJ. Whole-body imaging of thallium-201 after six different stress regimens. 35: 425-28
(4) J Nucl Med 1995; Hurwitz GA, et al. The VEX-test for myocardial scintigraphy with thallium-201 and sestamibi: effect on abdominal background activity. 36: 914-20
(5) Circulation 1989; Rossen JD, et al. Coronary dilation with standard dose dipyridamole and dipyridamole combined with handgrip. 79: 566-72
(6) J Nucl Med 1995; Czernin J, et al. Effects of modified pharmacologic stress approaches on hyperemic myocardial blood flow. 36: 575-80
(7) J Nucl Med 1994; Lalonde D, et al. Thallium-201-dipyridamole imaging: comparison between a standard dose and a high dose of dipyridamole in the detection of coronary artery disease. 35: 1245-53
(8) J Nucl Med 1989; Leppo JA. Dipyridamole-thallium imaging: the lazy man's stress test. 281-87
(9) J Nucl Med 1993; Whiting JH, et al. Cerebrovascular accident associated with dipyridamole thallium-201 myocardial imaging: case report. 34: 128-30
(10) J Nucl Med 1994; Schechter D, et al. Transient neurological events during dipyridamole stress test: an arterial steal phenomenon? 35: 1802-04
(11) J Nucl Med 1992; Allman KC, et al. Determination of extent and location of coronary artery disease in patients without prior myocardial infarction by thallium-201 tomography with pharmacologic stress. 33: 2067-73
(12) J Nucl Med 1995; Bottcher M, et al. Effect of caffeine on myocardial blood flow at rest and during pharmacological vasodilation. 36: 2016-21
(13) Nucl Med Annual 94, p.126-7
(14) Am J Cardiol 1988; Casale PN, et al. Simultaneous low level treadmill exercise and intravenous stress thallium imaging. 62: 799-802
(15) J Nucl Cardiol 2001; Vitola JV, et al. Exercise supplementation to dipyridamole prevents hypotension, improved electrocardiogram sensitivity, and increased heart-to-liver activity ratios on Tc-99m sestamibi imaging. 8: 652-59
(16) Am J Cardiol 2001; Leoncini M, et al. Prediction of functional recovery in patients with chronic coronary artery disease and left ventricular dysfunction combining the evaluation of myocardial perfusion and contractile reserve using nitrate-enhanced Tc-99m sestamibi gated single-photon emission computed tomography and dobutamine stress. 87: 1346-1350
(17) Am J Cardiol 2002; Leoncini M, et al. Usefulness of dobutamine Tc-99m sestamibi-gated single-photon emission computed tomography for prediction of left ventricular ejection fraction outcome after coronary revascularization for ischemic cardiomyopathy. 89: 817-821
(18) J Nucl Med 2002; Chin BB, et al. Myocardial contractile reserve and perfusion defect severity with rest and stress dobutamine 99mTc-sestamibi SPECT in canine stunning and subendocardial infarction. 43: 540-550
(19) J Nucl Cardiol 2002; Samady H, et al. Pharmacologic stress perfusion imaging with adenosine: Role of simultaneous low-level treadmill exercise. 9: 188-196
(20) J Nucl Med 2002; Ruiz M, et al. Arbutamine stress perfusion imaging in dogs with critical coronary artery stenosis: 99mTc-sestamibi versus 201Tl. 43: 664-670
(21) Radiographics 2002; Saremi F, et al. Pharmacologic interventions in nuclear radiology: indications, imaging protocols, and clinical results. 22: 477-490
(22) J Nucl Cardiol 2002; Simones MV, et al. Prediction of left ventricular wall motion recovery after acute myocardial infarction by Tl-201 gated SPECT: incremental value of integrated contractile reserve assessment. 9: 294-303
(23) J Nucl Med 2002; Schinkel AFL, et al. Prognostic value of dobutamine-atropine stress 99mTc-tetrofosmin myocardial perfusion SPECT in patients with known or suspected coronary artery disease. 43: 767-772
(24) J Nucl Cardiol 2002; Leoncini M, et al. Low-dose dobutamine nitrate-enhanced technetium 99m sestamibi gated SPECT versus low-dose dobutamine echocardiography for detecting reversible dysfunction in ischemic cardiomyopathy. 9: 402-406
(25) J Nucl Med Tech 2002; Zheng XM, Williams RC. Serum caffeine levels after 24-hour abstention: clinical implications on dipyridamole 201Tl myocardial perfusion imaging. 30: 123-127
(26) Radiology 2002; Schinkel AF, et al. Long term prognostic value of dobutamine stress 99mTc-sestamibi SPECT: single-center experience with 8-year follow-up. 225: 701-706
(27) J Nucl Med 2002; Elhendy A, et al. Dobutamine stress myocardial perfusion imaging in coronary artery disease. 43: 1634-1646
(28) J Nucl Cardiol 2003; Klodas E, et al. Prognostic significance of ischemic electrographic changes during vasodilator stress testing in patients with normal SPECT images. 10: 4-8
(29) J Nucl Cardiol 2003; Abbott BG, et al. Prognostic significance of ischemic electrocardiographic changes during adenosine infusion in patients with normal myocardial perfusion imaging. 10: 9-16
(30) J Nucl Cardiol 2003; Hendel RC, et al. Pharmacologic stress testing: new methods and new agents. 10: 197-204
(31) J Nucl Cardiol 2003; Holly TA, et al. The impact of adjunctive adenosine infusion during exercise myocardial myocardial perfusion imaging: results of both exercise and adenosine stress test (BEAST) trial. 10: 291-296
(32) J Nucl Cardiol 2003; Bottcher M, et al. Effect of antianginal medication on resting myocardial perfusion and pharmacologically induced hyperemia. 10: 345-52
(33) J Nucl Cardiol 2003; Beller GA. Clinical value of myocardial perfusion imaging in coronary artery disease. 10: 529-542
(34) J Ncul Med 2004; Kubo S, et al. Effect of caffeine intake on myocardial hyperemic flow induced by adenosine triphosphate and dipyridamole. 45: 730-738
(35) J Nucl Cardiol 2004; Travin MI, et al. The prognostic value of ECG-gated SPECT imaging in patients undergoing stress Tc-99m sestamibi myocardial perfusion imaging. 11: 253-262
(36) J Nucl Cardiol 2004; Lapeyre AC, et al. The impact of caffeine on vasodilator stress perfusion studies. 11: 506-511
(37) J Nucl Cardiol 2004; Druz RS, et al. Postischemic stunning after adenosine vasodilator stress. 11: 534-541
(38) J Nucl Cardiol 2004; Navare SM, et al. Comparison of risk stratification with pharmacologic and exercise stress myocardial perfusion imaging: a meta-analysis. 11: 551-561
(39) J Nucl Med 2005; Schinkel AFL, et al. Prognostic stratification using dobutamine stress 99mTc-tetrofosmin myocardial perfusion SPECT in elderly patients unable to perform exercise testing. 46: 12-18
(40) J Nucl Cardiol 2005; Lapeyre AC, et al. The prognostic value of pharmacologic stress myocardial perfusion imaging in patients with permanent pacemakers. 12: 37-42
(41) J Nucl Cardiol 2005; Barrett RJ, et al. Pharmacokinetcis and safety of biodenoson after intravenous dose escalation in healthy volunteers. 12: 166-171
(42) J Nucl Cardiol 2005; Cosmai EM, Heller GV. The clinical importance of electrocardiographic changes during pharmacologic stress testing with radionuclide myocardial perfusion imaging. 12: 466-472
(43) J Nucl Cardiol 2005; Giedd KN, et al. Sinus arrest during adenosine stress testing in liver transplant recipients with graft failure: three case reports and a review of the literature. 12: 696-702
(44) J Nucl Cardiol 2006; Hung GU, et al. Worsening of left ventricular ejection fraction induced by dipyridamole on Tl-201 gated myocardial perfusion imaging predicts significant coronary artery disease. 13: 225-232
(45) J Nucl Cardiol 2006; Jagathesan R, et al. Comparison of myocardial blood flow and coronary flow reserve during dobutamine and adenosine stress: implications for pharmacologic stress testing in coronary artery disease. 13: 324-32
(46) J Nucl Cardiol 2006; Boger LA, et al. Best patient preparation before and during radionuclide myocardial perfusion imaging studies. 13: 98-110
(47) J Nucl Cardiol 2007; Brunken RC. Challenges for measurement of myocardial perfusion and perfusion reserve by SPECT imaging. 14: 145-149
(48) J Nucl Cardiol 2007; Miyamoto MI, et al. Pharmacologic stress myocardial perfusion imaging: a practical approach. 250-255
(49) J Nucl Cardiol 2007; Iskandrian AE, et al. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: results of the ADVANCE phase 3 multicenter international trial. 14: 645-58
(50) J Nucl Cardiol 2007; Reyes E, et al. Side effect profile and tolerability of adenosine myocardial perfusion scintigraphy in patients with mild asthma or chronic obstrcutive pulmonary disease. 14: 827-834
(51) J Nucl Cardiol 2007; Mutlu H, Leppo J. Coronary steal and ST elevation during dipyridamole stress testing leading to coronary artery bypass grafting. 14: 892-897
(52) J Nucl Cardiol 2008; Bybee KA, Bateman TM. Symptom-limited exercise during vasodilator stress: best of both worlds? 15: 3-6
(53) J Nucl Cardiol 2008; Ahlberg AW, et al. Symptom-limited exercise combined with dipyridamole stress: prognostic value in assessment of known or suspected coronary artery disease by use of gated SPECT imaging. 15: 42-46
(54) J Nucl Cardiol 2008; Fricke E, et al. Respiratory resistance of patients during cardiac stress testing with adenosine: is dyspnea a sign of bronchospasm? 15: 94-99
(55) J Nucl Cardiol 2008; Di Carli MF, Hachamovitch R. Hybrid PET/CT is greater than the sum of its parts. 15: 118-122
(56) J Nucl Cardiol 2008; De Lorenzo A, Lima RSL. Influence of chronic renal failure on the heart rate response to dipyridamole in patients undergoing myocardial perfusion SPECT. 15: 193-200
(57) J Nucl Cardiol 2008; Lee JH, et al. Dobutamine-induced chest pain does not predict ischemic findings on myocardial perfusion imaging. 15: 526-529
(58) J Nucl Cardiol 2008; Thomas GS, et al. Safety of regadenoson, a selective adenosine A2A agonist, in patients with chronic obstrcutive pulmonary disease: a randomized double-blind, placebo-controlled trial (RegCOPD trial). 15: 319-328
(59) J Nucl Cardiol 2008; Leaker BR, et al. Safety of regadenoson, an adenosine receptor A2A agonist for myocardial perfusion imaging, in mild asthma and moderate asthma patients: a randomized, double-blinded, placebo-controlled trial. 15: 329-336
(60) J Nucl Cardiol 2008; Powles KE, et al. Practicing safe SPECT: caffeine abstinence in nuclear myocardial perfusion imaging. 15: 709-718
(61) J Nucl Cardiol 2009; Akutsu Y, et al. Delayed heart rate recovery after adenosine stress testing with supplemental arm exercise predicts mortality. 16: 54-62
(62) J Nucl Cardiol 2009; Thomas GS, et al. The RegEx trial: a randomized, double-blind, placebo- and active-controlled pilot study combining regadenoson, a selective A2A adenosine agonist, with low-level exercise, in patients undergoing myocardial perfusion imaging. 16: 63-72
(63) J Nucl Cardiol 2009; Yoon AJ, et al. The effect of beta-blockers on the diagnostic accuracy of vasodilator pharmacologic SPECT myocardial perfusion imaging. 16: 358-367
(64) J Nucl Cardiol 2009; Laighold S, Druz R. Initial clinical experience with a selective A2A receptor agonist, regadenoson, in a patient with end-stage renal disease on hemodialysis. 16: 478-480
(65) J Nucl Cardiol 2009; Bart BA, et al. Comparison of dobutamine stress echocardiography, dobutamine SPECT, and adenosine SPECT myocardial perfusion imaging in patients with end-stage renal disease. 16: 507-515
(66) J Nucl Cardiol 2010; Gemignani AS, Abbott BG. The emerging role of the selective A2A agonist in pharmacologic stress testing. 17: 494-497
(67) J Nucl Med 2010; Reyes E, et al. Attenuation of adenosine-induced myocardial perfusion heterogeneity by atenolol and other cardioselective β-adrenoceptor blockers: a crossover myocardial perfusion imaging study. 51: 1036-1043
(68) J Nucl Cardiol 2010; Hage FG, Iskandrian AE. Heart rate response during vasodilator stress myocardial perfusion imaging: mechanisms and implications. 17: 617-624
(69) J Nucl Cardiol 2010; Schelbert HR. Anatomy and physiology of coronary blood flow. 17: 545-554
(70) J Nucl Cardiol 2010; Mathur S, et al. Blunted heart rate response as a predictor of cardiac death in patients undergoing vasodilator stress technetium-99m sestamibi gated SPECT myocardial perfusion imaging. 17: 617-624
(71) J Nucl Cardiol 2010; Kwon DH, et al. Lessons from regadenoson and low-level tredmill/regadenoson myocardial perfusion imaging: initial clinical experience in 1263 patients. 17: 853-857
(72) J Nucl Cardiol 2010; Sharma J, et al. Patients with adenosine-induced ST-segment depressions and normal myocardial perfusion imaging: cardiac outcomes at 24 months. 17: 874-880
(73) J Nucl Cardiol 2011; Rozanski A, et al. Comparison of long-term mortality risk following normal exercise vs adenosine myocardial perfusion SPECT. 17: 999-1008
(74) J Nucl Cardiol 2011; Tejani FH, et al. Effect of caffeine on SPECT myocardial perfusion imaging during regadenoson pharmacologic stress: rationale and design of a prospective, randomized, multicenter study. 18: 73-81
(75) J Nucl Cardiol 2011; Aljaroudi W, et al. Safety of
regadenoson in patients with end-stage liver disease. 18: 90-95
(76) J Nucl Cardiol 2011; Fine NM, Pellikka PA. Stress
echocardiography for the detection and assessment of coronary
artery disease. 18: 501-515
(77) J Nucl Cardiol 2011; Grady EC, et al. Development of
asystole requiring cardiac resuscitation after the administration
of regadenoson in a patient with pulmonary fibrosis receiving
n-acetylcysteine. 18: 521-525
(78) J Nucl Cardiol 2011; Palani G, et al. Safety of regadenoson
as a pharmacologic stress agent for myocardial perfusion imaging
in chronic kidney disease patients not on dialysis. 18: 605-611
(79) J Nucl Cardiol 2011; Reyes E, et al. Effect of body mass on
the efficacy, side effect profile, and plasma concentration of
fixed-dose regadenoson for myocardial perfusion imaging. 18:
620-627
(80) J Nucl Cardiol 2011; Cavalcante JL, et al. Regadenoson is a
safe and well-toerlated pharmacological stress agent for
myocardial perfusion imaging in post-heart transplant patients.
18: 628-633
(81) J Nucl Cardiol 2011; Hage FG, et al. A blunted heart rate
response to regadenoson is an independent prognostic indicator in
patients undergoing myocardial perfusion imaging. 18: 1086-1094
(82) J Nucl Cardiol 2012; Abbott BG. The vasodilator stress ECG:
should depression cause anxiety? 19: 13-15
(83) J Nucl Cardiol 2012; Azemi T, et al. Electrocardiographic
changes during vasodilator SPECT myocardial perfusion imaging:
does it affect diagnosis or prognosis? 19: 84-91
(84) J Nucl Cardiol 2012; Zhao G, et al. Selective action of
metoprolol to attenuate regadenoson-induced tachycardia in
conscious dogs. 19: 109-17
(85) J Nucl Cardiol 2012; Zoghbi GJ, Iskandrian AE. Selective
adenosine agonists and myocardial perfusion imaging. 19: 126-141
(86) J Nucl Cardiol 2012; DePuey EG, et al. Patient-centered
imaging. 19: 185-215
(87) J Nucl Cardiol 2012; Ananthasubramaniam K, et al. A
randomized, double-blind, placebo-controlled study of the safety
and tolerance of regadenoson in subjects with stage 3 or 4 chronic
kidney disease. 19: 319-329
(88) J Nucl Cardiol 2012; Page RL, et al. Seizures associated
with regadenoson: a case series. 19: 389-391
(89) J Nucl Cardiol 2012; Hage FG, Iskandrian AE. The effect of
caffience on adenosine myocardial perfusion imaging: time to
reassess? 1: 415-419
(90) J Nucl Cardiol 2012; Attenuation of the side effect profile
of readenoson: a randominzed double-blinded placebo-controlled
study with aminophylline in patients undergoing myocardial
perfusion imaging. The ASSUAGE trial. 19: 448-457
(91) J Nucl Cardiol 2012; Lee JC, et al. Effect of caffeine on
adenosine-induced reversible perfusion defects assessed by
automated analysis. 19: 474-481
(92) J Nucl Cardiol 2012; Prenner BM, et al. A randomized,
double-blind, placebo-controlled study assessing the safety and
tolerability of regadenoson in sibjects with asthma or chronic
obstructive pulmonary disease. 19: 681-692
(93) J Nucl Cardiol 2012; Katz JS, et al. Assessment of transient
ischemic dilatation (TID) ratio in gated SPECT myocardial
perfusion imaging (MPI) using regadenoson, a new agent for
pharmacologic stress testing. 19: 727-734
(94) J Nucl Cardiol 2012; Emmett L, et al. Comparative assessment
of rest and post-stress left ventricular volumes and left
ventricular ejection fraction on gated myocardial perfusion
imaging (MPI) and echocardiography in patients with transient
ischemic dilatation on adenosine MPI: myocardial stunning or
subendocardial hypoperfusion? 19: 735-742
(95) J Nucl Cardiol 2012; Thomas GS, et al. Advanced hybrid
stress testing: a potential new paradigm combining exercise and
pharmacologic stress. 19: 887-890
(96) J Nucl Cardiol 2012; Partington SL, et al. SAfety and feasibility of regadenoson use for suboptimal heart rate response during symptom-limited standard Bruce exercise stress test. 19: 970-978
(97) J Nucl Cardiol 2012; Shaw LJ, et al. Prognosis in the era of
comparative effectiveness research: where is nuclear cardiology
now and where should it be? 19: 1026-1043
(98) J Nucl Cardiol 2012; Gupta A, et al. QTc prolongation after
regadenoson administration. 19: 1080-1082
(99) J Nucl Cardiol 2012; Pandit A, Freiman SU. Complete heart
block associated with regadenoson: a real side effect. 19:
1236-1239
(100) J Nucl Cardiol 2013; Cullom SJ, et al. Regadenoson
pharmacologic rubidium-82 PET: a comparison of quantitative
perfusion and function to dipyridamole. 20: 76-83
(101) J Nucl Cardiol 2013; Parker MW, et al. A strategy of
symptom-limited exercise with regadenoson-as-needed for stress
myocardial perfusion imaging: a randomized controlled trial. 20:
185-196
(102) J Nucl Cardiol 2013; Ross MI, et al. Safety and feasibility
of adjunctive regadenoson injection at peak exercise dueing
exercise myocardial perfusion imaging: the both exercise and
regadenoson stress test (BERST) trial. 20: 197-204
(103) J Nucl Cardiol 2013; Doukky R, et al. The safety and
tolerability of regadenoson in patients with end-stage renal
disease: the first prospective evaluation. 20: 205-213
(104) J Nucl Cardiol 2013; Thompson RC, et al. Regadenoson
pharmacologic stress for myocardial perfusion imaging: a three-way
comparison between regadenoson administered at peak exercise,
during walk recovery, or no-exercise. 20: 214-221
(105) J Nucl Cardiol 2013; Regadenoson: a focused update. 20:
284-288
(106) J Nucl Cardiol 2013; Thomas GS, et al. Is regadenoson an
appropriate stressor for MPI in patient with left bundle branch
block or pacemakers? 20: 1076-1085
(107) J Nucl Cardiol 2014; Bellam N, et al. Prognostic
significance of impaired chronotropic response to pharmacologic
stress Rb-82 PET. 21: 233-244
(108) J Nucl Cardiol 2014; Rosenblatt J, et al. Asystole
following regadenoson infusion in stable outpatients. 21: 862-868
(109) J Nucl Cardiol 2014; Agarwal V, DePuey EG. Regadenoson and
seizures: a real clinical concern. 21: 869-870
(110) J Nucl Cardiol 2014; Hage FG, Iskandrian AE. Serious
complications associated with regadenoson administration for
myocardial perfusion imaging: a commentary. 21: 877-879
(111) J Nucl Cardiol 2014; Hoffmeister C, et al The effect of
beta blocker withdrawl on adenosine myocardial perfusion imaging.
21: 1223-1229
(112) J Nucl Cardiol 2015; Golzar Y, et al. The significance of
automatically measured transient ischemic dilatation in
identifying severe and extensive coronary artery disease in
regadenoson, single-isotope technetium-99m myocardial perfusion
SPECT. 22: 526-534
(113) J Nucl Cardiol 2015; Farzaneh-Far A, et al. Comparison of
the prognostic value of regadenoson and adenosine myocardial
perfusion imaging. 22: 600-607
(114) J Nucl Cardiol 2015; Doukky R. The prognostic value of
regadenoson stress: has the case been made? 22: 608-610
(115) J Nucl Cardiol 2015; Doukky R, et al. Diagnostic and
prognostic significance of ischemic electrocardiograhic changes
with regadenoson-stress myocardial perfusion imaging. 22: 700-713
(116) J Nucl Cardiol 2015; Hage FG, et al. Review of
cardiovascular imaging in The Journal of Nuclear Cardiology in
2014: Part 3 of 2: myocardial perfusion imaging. 22: 714-719
(117) J Nucl Cardiol 2015; Rangel MO, et al. Severe chronic
kidney disease as a predictor of benefit from aminophylline
administration in patients undergoing regadenoson stress
myocardial perfusion imaging: A substudy of the ASSUAGE and
ASSUAGE-CKD trials. 22: 1008-1018
(118) J Nucl Cardiol 2015; Dilsizian V, et al. Serious and
potentially life threatening complications of cardiac stress
testing: physiological mechanisms and management strategies. 22:
1198-1213
(119) J Nucl Cardiol 2015; Hage FG, et al. The prognostic value
of regadenoson myocardial perfusion imaging. 22: 1214-1221
(120) J Nucl Cardiol 2015; Acampa W, et al. Prognostication in
the era of a new stressor for myocardial perfusion imaging. 22:
1222-1224
(121) J Nucl Cardiol 2016; Poulin MF, et al. Prognostic
implications of stress modality on mortality risk and cause of
death in patients undergoing office-based SPECT myocardial
perfusion imaging. 23: 202-211
(122) J Nucl Cardiol 2016; Uretsky S. Beyond ischemia evaluation:
the potential for assessing and addressing physical inactivity in
the cardiac stress laboratory. 23: 212-214
(123) J Nucl Cardiol 2016; Bajaj NS, et al. The prognostic value
of non-perfusion variables obtained during vasodilator stress
myocardial perfusion imaging. 23: 390-413
(124) J Nucl Cardiol 2016; Aljaroudi W, et al. Prognostic value of heart rate response during regadenoson stress myocardial perfusion imaging in patients with end stage renal disease. 23: 560-569
(125) J Nucl Cardiol 2016; Hage FG, et al. Review of
cardiovascular imaging in the Journal of Nuclear Cardiology in
2015- Part 2 of 2: myocardial perfusion imaging. 23: 493-498
(126) J Nucl Cardiol 2016; Andrikopoulou E, Hage FG. Heart rate
response to regadenoson: making the case for its value in clinical
practice. 23: 575-580
(127) J Nucl Cardiol 2016; Henzlova M, et al. ASNC imaging
guidelines for SPECT nuclear cardiology procedures: stress,
protocols, and tracers. 23: 606-639
(128) J Nucl Cardiol 2016; Jovin IS, et al. The influence of
clopidogrel on ischemia diagnosed by myocardial perfusion stress
testing. 23: 773-779
(129) J Nucl Cardiol 2016; Platsman Z, et al. Regadenoson-induced
coronary vasospasm resulting in severe reversible perfusion
defects and transient ischemic dilatation on SPECT stress
myocardial perfusion imaging. 23: 843-845
(130) J Nucl Cardiol 2016; Lester D, et al. Prognostic value of
transient ischemia dilatation with regadenoson myocardial
perfusion imaging. 23: 1147-1155
(131) J Nucl Cardiol 2016; Loffler AI, Bourque JM. Prognostic
impact of TID in regadenoson MPI: some patients and certain
events. 23: 1156-1159
(132) J Nucl Cardiol 2017; Thomas GS, et al. When to re-dose
regadenoson? 24: 66-68
(133) J Nucl Cardiol 2017; Doukky R, et al. The prognostic value
of regadenoson SPECT myocardial perfusion imaging in patients with
end-stage renal disease. 24: 112-118
(134) J Nucl Cardiol 2017; Miller EO, Schwartz RG. Cardiovascular
risk assessment with regadenoson SPECT MPI in patients with
end-stage renal disease is safe, effective, and well tolerated:
does is matter? 24: 119-121
(135) J Nucl Cardiol 2017; Massalha S, et al. Conduction
abnormalities during dipyridamole stress testing. 24: 405-409
(136) J Nucl Cardiol 2017; Subbiah R, Patil PV. Arrhythmias in
vasodilator stress testing. 24: 410-412
(137) J Nucl Cardiol 2017; Saab R, et al. Vasodilator stress
agents for myocardial perfusion imaging. 24: 434-438
(138) J Nucl Cardiol 2017; Thomas GS, et al. The EXERRT trial:
"EXErcise to regadenoson in recovery trial": A phase 3b,
open-label, parallel group, randomized, multicenter study to
assess regadenoson administration following an inadequate exercise
stress test as compared to regadenoson without exercise for
myocardial perfusion imaging using a SPECT protocol. 24: 788-802
(139) J Nucl Cardiol 2017; Doran JA, et al. Aminophylline and
caffeine for reversal of adverse symptoms associated with
regadenoson SPECT MPI. 24: 1062-1070
(140) J Nucl Cardiol 2017; Hage FG, Aljaroudi WA. Review of
cardiovascular imaging in the journal of nuclear cardiology in
2016: part 2 of 2- myocardial perfusion imaging. 24: 1190-1199
(141) J Nucl Cardiol 2017; Hussalin N, et al. An assessment of
the safety, hemodynamic response, and diagnostic accuracy of
commonly used vasodilator stressors in patients with severe aortic
stenosis. 24: 1200-1213
(142) J Nucl Cardiol 2017; Fughhi I, et al. Impact of regimented
aminophylline administration protocol on the burden of
regadenoson-induced ischemia detected by SPECT myocardial
perfusion imaging. 24: 1571-1578
(143) J Nucl Cardiol 2017; Thompson RC, Thomas GS. The EXXERT
study. 24: 1800-1802
(144) J Nucl Cardiol 2017; Kureshi F, et al. Regadenoson-induced
complete heart block and asystole: a real possibility nuclear
laboratories should be aware of. 24: 2019-2024