MRI shows that first responders to the September 11 terrorist attacks who later had post-traumatic stress disorder (PTSD) are at higher risk of cognitive impairment as they age, according to research presented at the International Society for Magnetic Resonance in Medicine (ISMRM) meeting.
The study shows that first responders to the World Trade Center attack experienced negative long-term effects, said presenter Juin Zhou, PhD, of Stony Brook University in New York.
"After the collapse of the World Trade Center, there was an extensive search and rescue effort that exposed responders to emotionally, mentally, and physically taxing conditions," she said. "Two decades later, as they approach midlife, 22% have chronic PTSD, [which is a rate] higher than the general population."
ISMRM is holding this week's meeting in conjunction with the European Society for Magnetic Resonance in Medicine and Biology and the International Society for MR Radiographers and Technologists.
Questions about PTSD and brain health
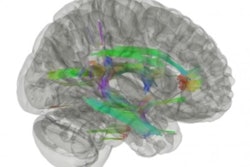
Many of the responders to the World Trade Center attack are now middle-aged, and almost a quarter are experiencing PTSD as well as mild cognitive impairment (MCI), which can be a precursor to Alzheimer's disease, Zhou and colleagues noted in their abstract. Previous research has shown that the white-matter connectivity of these responders with MCI differs from their unimpaired counterparts, but the effects of PTSD on brain health in this population have not been thoroughly investigated.
Using diffusion MRI, the group analyzed 97 responders to the World Trade Center attacks who were diagnosed with and without cognitive impairment and/or PTSD (49 of these were cognitively impaired). Study participants were categorized as cognitively impaired or unimpaired using the Montreal Cognitive Assessment (MoCA) too; scores range from 0 to 30, with those over 26 indicating a healthy brain. Of the 49 cognitively impaired study participants, 24 were also diagnosed with PTSD.
Zhou and colleagues found that responders with World Trade Center-related PTSD have higher incidence of MCI, as well as reduced white-matter connectivity in eight particular "tract bundles," primarily in the limbic system, along the cingulum -- the latter being a finding consistent with previous studies that have shown abnormalities in the limbic pathway to be linked with cognitive impairment in multiple sclerosis, Parkinson's disease, and Alzheimer's.
Zhou listed the white-matter bundles that showed reduced connectivity in cognitively impaired World Trade Center responders with PTSD:
- Left and right fornix
- Corpus callosum forceps major
- Right arcuate fasciculus
- Right cingulum frontal parietal
- Left and right cingulum rarolfactory
- Left cingulum frontal parahippocampal
- Corpus callosum forceps minor
"In contrast to cognitively unimpaired responders with PTSD, individuals with both PTSD and cognitive impairment also present with reduced connectivity in the limbic system, [and] regions along the cingulum bundle also present with decreased fractional anisotropy," she and colleagues noted.
PTSD appears to alter the progression of cognitive impairment in the World Trade Center responder population, they concluded.
"The results of this study improve our understanding of cognitive impairment disease unique to World Trade Center responders and could influence treatment [decisions for] these patients," Zhou told session attendees.