The use of even small amounts of cannabis can cause changes in the brains of adolescents, according to recent studies using MRI. The findings indicate that researchers should pay close attention to increasing cannabis use, especially in vulnerable populations, according to a presentation last week at the Society for Magnetic Resonance Radiographers & Technologists (SMRT) meeting.
Studies have shown that adolescents who use marijuana just once or twice experience brain changes that show up on MRI compared with individuals who do not use cannabis. This indicates that cannabis may not be completely harmless, especially for some individuals.
"The predominant pattern of use is occasional and nonproblematic," said Scott Mackey, PhD, of the department of psychiatry at the University of Vermont in Burlington. "But a considerable portion, about 20% of those who are regular users, will go on to have periods of disordered use at some point in their life."
Permissive attitudes about cannabis use
A more permissive societal outlook about the use of cannabis has led to expanded legalization of the substance across the U.S. and Canada. Data show that close to 35% of U.S. students in grade 10 have reported using cannabis.
But imaging studies of cannabis users have demonstrated that in the adolescent period, the brain, not yet fully developed, may be particularly at risk for the effects of delta-9-tetrahydrocannabinol (THC) on its structure, Mackey warned.
He cited three specific populations that are potentially at greater risk of being adversely affected by cannabis use: those with a predisposition for substance use disorder, adolescents, and patients with schizophrenia or other psychotic disorders.
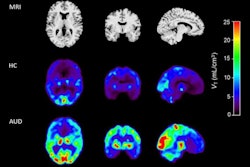
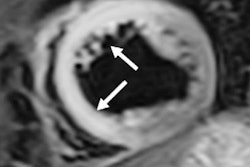
A study published March 6 in the Journal of Neuroscience by Orr and colleagues used MRI with a voxel-based morphometry technique to analyze the brains of 46 adolescents with very low levels of exposure to cannabis and compared them with individuals with no exposure to THC. MRI found that gray-matter volume was altered in relation to early exposure to cannabis in several parts of the brain that have greater expression of CB1 receptors.
"There was an impact on the striatum and the insula in 14-year-olds who only had one or two exposures to marijuana," said Mackey, one of the study's authors. "Since this effect was not seen in a separate group of adolescents who had one or two exposures by the age of 16, it looks as if exposure, even very little exposure, to cannabis before the age of 14 may have significant toxic effects."
Little research has been conducted in adolescents with respect to cannabis use, specifically in adolescents who have used cannabis sparsely.
Mackey described recent results from the Enhancing Neuro Imaging Genetics Through Meta-Analysis (ENIGMA) Addiction consortium on adults diagnosed with substance dependence. In the largest neuroimaging study of addiction to date, combining data from more than 30 labs around the world, the consortium found a common set of five brain regions with lower volume in dependent substance users compared with nondependent controls, regardless of the substance used.
"It is a remarkable finding that dependence on cannabis appears to involve brain differences in the same regions that are seen in dependence on nicotine, alcohol, cocaine, and methamphetamine," Mackey said.
The size of these effects, however, is very small, so they would not be observable in individual brain scans.
"You cannot tell which individuals are regular cannabis users just by looking at their structural brain scans," he explained. "These are group-level differences."
Cannabis and psychosis
Adolescent cannabis use is a well-known risk factor for psychosis; cannabis use in adults with a history of psychosis is a risk factor for relapse of psychosis; and exposure to cannabis can produce mild psychotic symptoms, such as paranoia, in healthy volunteers, according to Mackey. It's not known, though, whether cannabis use is the cause of these outcomes or if these are the result of another underlying factor such as early adversity, stress, or a genetic predisposition toward dopamine dysregulation, he added.
Individuals with schizophrenia are at particularly high risk of developing substance use disorder, and the drug they are most likely to become addicted to is cannabis, Mackey noted. It's problematic when a patient with schizophrenia develops cannabis use disorder because it can interfere with the management of schizophrenia.
One possible explanation for why cannabis use is so prevalent among patients with schizophrenia is that their drug therapies, usually atypical antipsychotic agents, disrupt dopaminergic transmission, which may, in part, be restored by cannabis use -- making cannabis use a form of self-medication in patients with schizophrenia.
"They may be using marijuana to counterbalance the antipsychotic medications that they are on," Mackey said, explaining that the medications treat the positive symptoms associated with schizophrenia, such as delusions and hallucinations.
A possible recommendation could be to make cannabis with a reduced amount of THC available for populations that are at greater risk for cannabis-related psychosis, including individuals with schizophrenia, he said.
Further study is necessary to better understand the impact of cannabis use on populations that are at elevated risk for adverse effects from continued usage, Mackey said.
"It is precisely now, when the movement to legalize cannabis is sweeping across the continent, that we need more research to inform our decision-making about the regulation of cannabis," he said.