VIENNA - Chronic low back pain is the most common cause of disability between the ages of 45 and 65, which means that it is something radiologists will have to deal with during their careers. When they do, they should be able to read films properly.
But reading films alone will not be enough to make the correct diagnosis, and an image without clinical examination is nothing, according to Dr. Afshin Gangi, PhD, the chairman of radiology and nuclear medicine at the University Hospital of Strasbourg in France, who chaired the dedicated Refresher Course on Saturday.
 Dr. Afshin Gangi, PhD, from Strasbourg, France.
Dr. Afshin Gangi, PhD, from Strasbourg, France."Please don't report anything without having seen the patient first. When the clinical examination is not consistent with what you see, you should report it exactly like this, it's extremely important. Imaging alone, without clinical examination, is not telling you anything, the pain could be anywhere. Examine your patient, read the film at the same time, then suggest what to do. The pain could have multiple causes," he said.
Dr. David Wilson, a consultant radiologist at BMI Healthcare Oxford Clinic in the U.K., agreed. "The moment you start to use the imaging criteria as your end point, you'll start making mistakes," he said to a packed audience.
In his talk, Wilson focused on sacroiliac joint syndrome, a condition with a considerable amount of pain and poor clinical signs. He stressed the role of interventional procedures in the diagnosis and treatment of this condition.
Radiologists first need to remember that the anatomy of the region is complicated. "The joint has an almost S shape, it is curving like a snake in two directions," he said. Part of the joint is fibrocartilage and hyaline cartilage, a solid structure that does allow some flexibility. Ligamental structures in this area are complex, deep, and thick. "Those of you doing interventional procedures in these areas will be passing your needles through very thick fibrous material before you get down to the joint," he said.
 Dr. David Wilson from Oxford, U.K.
Dr. David Wilson from Oxford, U.K.The clinical signs of sacroiliac joint syndrome include localized tenderness, compression across the pelvis, and distraction. "All of these are techniques that physiotherapists, rheumatologists, and surgeons may be using, and they may become convinced that these are excellent techniques. But, sadly, evidence in literature shows the exact opposite," he pointed out.
These tests have very poor predictive value, and there is no single test that is consistently valid, according to Wilson. A clinical examination alone is clearly not enough then.
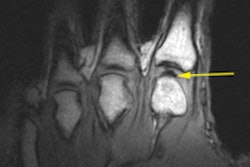
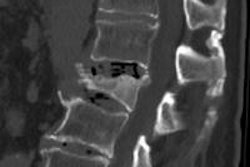
Imaging can help in the assessment of the syndrome. With a sensitivity of 85%, MRI seems to be the most appropriate tool. Conventional radiographs have poor sensitivity and should not be used except for trauma. CT is particularly good at detecting erosions and inflammation, but, unlike MRI, it does not show bone edema, one of the earliest signs of the disease. SPECT has a modest sensitivity of 46% to 72%, and there is only limited data on PET.
Some patients have mechanical problems, which will not show on imaging. Patients with severe chronic pain do not require an imaging examination. In these cases, radiologists can do tests to assess the origin of the pain and then try to block it. For this, they need to place a needle directly into the joint to inject a steroid/anesthetic mixture.
"This is tricky because of the anatomy of the joint. We all have problems with it," Wilson said. The needle has to take different angles according to which point one attacks. Image guidance is crucial in that area, and blind injection is, with a 15% accuracy of placement, "even worse than tossing a coin."
There is some debate around the use of ultrasound, but it has yielded poor results to date with 40% accuracy of placement.
Up until two years ago, Wilson used fluoroscopy. Unfortunately, things did not always go well. "Extravasations are very common; they represent about 60% of the attempts we have made."
The problem with CT is the radiation involved, as there needs to be both front and rear examinations. Fusion CT or MR with ultrasound may be the answer. "Sacroiliac joint imaging is now almost like cheating. I can put the needle in the joint without feeling the edges. I've never done that before, it's great, it doesn't irradiate the patient or me."
Originally published in ECR Today on 9 March 2014.
Copyright © 2014 European Society of Radiology