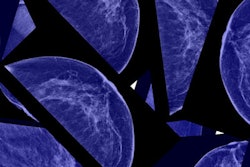
CHICAGO - One in five women say they would likely skip additional imaging after an abnormal mammogram due to out-of-pocket costs, according to a study presented November 29 at RSNA 2022 in Chicago.
 Dr. Michael Ngo.
Dr. Michael Ngo.In a survey of patients presenting for initial breast cancer screening, researchers led by Dr. Michael Ngo of Boston Medical Center found 21% of respondents said they would skip further imaging if they knew they had to pay a deductible.
"Our study demonstrates that out-of-pocket payments will discourage people, especially those belonging in the most vulnerable populations, from completing the last steps in the breast cancer screening process," Ngo said in an RSNA news release.
Anecdotal reports suggest that since the Affordable Care Act (ACA) was enacted in 2010, some breast imaging practices have seen a decline in patient adherence to recommended follow-up imaging after an abnormal initial mammography result, according to the authors. The ACA removed out-of-pocket costs for screening mammograms under most health plans but does not cover costs for additional imaging or biopsy.
"Prior studies have shown that out-of-pocket costs deter patients from attending screening mammography," Ngo said.
To explore the issue, the researchers surveyed 932 patients at their hospital between September 2021 and February 2022 with a questionnaire that included demographic questions (race, education level, annual household income, and insurer) as well as scenarios about the utilization of breast imaging.
When asked if they would skip indicated imaging if they knew they had to pay a deductible, 151 out of 714 respondents (21.2%) said they would skip imaging, 424 (59.4%) said they would not, and 139 (19.5%) were undecided.
Of even more concern, groups with the highest percentage of responses indicating they would skip additional imaging were Latinx (33%), high school educated or less (31%), patients with a household income less than $35,000 (27%), and Medicaid/uninsured patients (31.5%).
"These results could be used to advocate for legislation that will cover these important follow-up tests and prevent further exacerbation of existing health inequities," Ngo said.