Mistakes made during initial reads can be spun into a learning experience for residents, according to researchers from the University of Pittsburgh. They assessed the most frequent interpretation errors made by on-call residents at their institution.
"Overnight emergency department radiology coverage results in preliminary readings that occasionally differ from final interpretations," wrote Dr. Barton Branstetter IV and colleagues in their 2005 RSNA poster presentation in Chicago. "On-call residents would benefit from understanding the most common misinterpretations ... so that they can more critically examine areas where errors are frequent."
The data for this study was collected from the group's academic medical center consisting of one main hospital and 19 specialty and community satellites. A little over a million radiology reports are generated per year with preliminary reports fed directly into the PACS, which can be accessed from any workstation. Each preliminary report was reviewed at the time of final interpretation, and significant discrepancies -- defined as a "difference in interpretation that could immediately change patient management -- were recorded electronically.
The million-plus cases were narrowed down to 612,890, and the error types were classified as overcalled, undercalled, or misinterpreted. The authors pinpointed 3,194 instances of significant discrepancy (0.52% error rate) that were then categorized into four organ system categories: neuroradiology (0.35% error rate), musculoskeletal (0.77% error rate), thoracic (0.62% error rate), and abdominal (0.43% error rate).
In neuroradiology, stroke was most often misinterpreted or undercalled (22% of cases). In musculoskeletal imaging, leg fractures were misinterpreted or undercalled (51%). In abdominal imaging, leaks and inflammation were missed or undercalled most often (25%).
In thoracic imaging, confusion between congestive heart failure and pneumonia predominated, with 28% of pneumonia cases missed. The authors singled out one case in which a nodule was missed under the right fourth rib on x-ray. They mentioned that the teaching point that can be gleaned from these misinterpreted chest cases was that residents should "avoid satisfaction of search. A full survey should be completed even when a study is ordered for a specific purpose, such a placement of a PICC line in this case."
 |
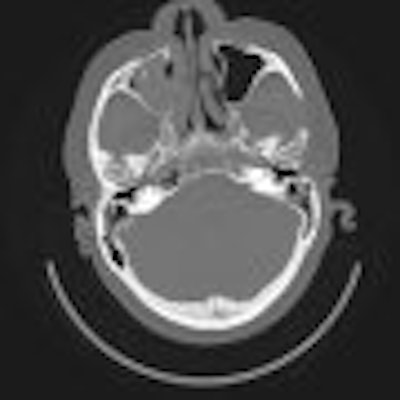
| A right orbital floor fracture that was missed. Ancillary findings should increase suspicion for specific pathology. Blood in a maxillary sinus is a finding on axial images that is highly suspicious for an orbital floor fracture. The fracture itself may be difficult to discern because it is in the plane of imaging. Images courtesy of Dr. Barton Branstetter IV. |
 |
An electronic preliminary report generator (PRG) can serve as a useful teaching tool by giving trainees the chance to review mistakes and prevent the same errors in the future, they concluded.
In a follow-up interview with AuntMinnie.com, Branstetter -- who is the director of head and neck imaging, as well as the associate director of radiology informatics at the university -- shared additional information from this research.
Did you find any differences in the error rates among residents depending on what year they were in?
We didn't formally break down error rates by year in residency.... Our residents start taking ER call six months into their residency, and they continue for a year before being graduated to senior call. Thus the vast majority of the discrepancies in our study would be from residents in the latter half of their first year and the first half of their second year.
At your institution, do you have a program in place (lectures, conferences, self-study teaching files, etc.) through which residents can review errors?
The software that we used to track the discrepancies (PRG) is also our formal feedback mechanism. Whenever a significant discordance is registered, an e-mail is sent to the resident who made the error asking him to re-examine the case.
Furthermore, our PACS makes it easy to save cases in a work list so most residents set up a list of every case they see on-call. Then they can return to that list at their leisure to see what they got right and what they got wrong.
This mechanism was designed to allow postcall residents to leave the hospital at the end of their shift, instead of going over all their cases with attendings in the morning. That way the resident can receive the feedback when they are less sleep-deprived. Of course, there are always a few cases of such great interest that the resident couldn't even sleep without knowing what the right answer is, so they still often drop by the reading room on the way out.
In addition, noon conferences are regularly set aside for review of missed cases, so that all the residents can benefit from their colleagues' mistakes.
Do you plan to continue tracking preliminary error reports to see if there have been changes or improvements because of this review system?
Although the system would allow us to do so, we don't track individual performance over time. Also, we haven't analyzed our discrepancy rates over time to see if the PRG is improving our rates.
One of the major take-home points that we tried to communicate in our presentation was how effective the PRG software is as a teaching tool and as a quality assurance tool. We've been using ours since 1998, and, with over 650,000 cases, we have a tremendous amount of experience to build upon.
By Shalmali Pal
AuntMinnie.com staff writer
December 22, 2005
Related Reading
Computerized physician order entry system linked with increased patient mortality, December 7, 2005
Most rad residents OK with on-call preparation, duty, November 14, 2005
Medical errors edging up in U.S., study finds, May 2, 2005
Copyright © 2005 AuntMinnie.com