Patients can significantly reduce the length of time that they have to hold their breath without affecting image quality during PET/CT-guided percutaneous liver biopsies or ablations, according to a study presented at the annual meeting of the Society of Interventional Radiology (SIR) in San Francisco.
The benefits of the shorter breath-holds are reduced procedure times and less anesthesia for patients, as well as improved image registration between CT and PET images with no compromise in accuracy for interventional radiologists, according to researchers from Brigham and Women's Hospital in Boston.
"Because we can often use PET/CT with only 20-second PET acquisition, it makes it easier to do breath-hold techniques, which will improve image registration between CT and PET and that will improve targeting [of lesions]," said study co-author Dr. Paul B. Shyn from the department of abdominal imaging and intervention at Brigham and Women's Hospital. "This idea should work pretty much anywhere in the body."
Organs in motion
One of the challenges in image-guided liver biopsies and ablations is that the organ is in motion as the patient breathes. When using PET/CT, particularly if the lesion is not seen well on CT, interventional radiologists need to know the metabolic activity is in the right place relative to the CT image every time, Shyn explained to AuntMinnie.com.
A patient usually can hold his or her breath without difficulty for a CT scan, because imaging time is relatively short. However, PET typically requires continuous breathing, because image acquisition takes from one to five minutes per bed position.
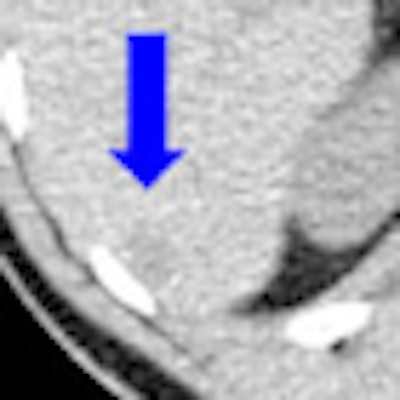
"Inherently, that means that structures that are moving with breathing will be subject to misregistration, and the CT image may not line up with the PET image," Shyn said. "With PET, longer acquisitions with breathing also can cause some distortion of the lesion. In other words, with respiratory motion the lesion may appear to be longer in the z-axis, because it is moving in that direction with each respiratory cycle."
He added that the CT image, whether it is done with a breath-hold or as quiet breathing, also may be "a little unpredictable" in detailing the lesion's spatial localization relative to the PET image.
"Right now, I think it is a minority of cases where PET/CT adds to these biopsies and ablation procedures, but there are cases where it [adds information]," Shyn said. "Those are cases where we do not see the lesion well on CT, and having the FDG uptake [on PET] makes much more clear what we are going after."
Imaging protocols
Shyn and colleagues studied 10 patients (seven females and three males, ranging in age from 39 to 78 years) with 13 liver lesions that were visible on FDG-PET and unenhanced CT scans (Discovery VCT, GE Healthcare).
Five patients underwent percutaneous PET/CT-guided radiofrequency ablation (two patients) or cryoablation (three patients). In addition, five other patients underwent diagnostic PET/CT-guided percutaneous fine-needle aspiration biopsy.
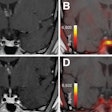
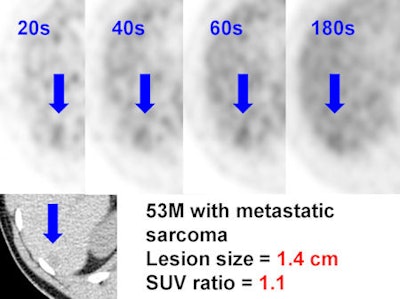
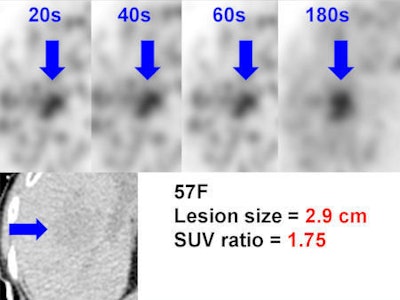
Patients performed one breath-hold during the CT scan and nine breath-holds, beginning 20 seconds into the study, to acquire the PET images. The researchers then reconstructed the PET scans for each patient at 20 seconds, 40 seconds, 60 seconds, and 180 seconds.
Two interventional radiologists randomly reviewed 40 PET datasets followed by 10 CT datasets and marked the centers of the tumors. They calculated the distance of the errors in target localization for each PET dataset and used PET and CT images acquired at 180 seconds as the gold standard for evaluation. Tumor sizes and tumor FDG avidities were correlated with magnitudes of targeting errors.
The analysis found that targeting errors for PET images at 20 seconds compared to PET images at 180 seconds ranged from 0.74 to 64.3 mm, with a mean error distance of 13.2 mm. Targeting errors for PET at 20 seconds were "not significantly different" than targeting errors for PET at 40 seconds (0.93 mm) and at 60 seconds (0.38 mm).
Targeting errors
In addition, 20-second PET targeting errors compared to CT ranged from 0.64 to 64.8 mm, with a mean of 17.3 mm. Again, those results were "not statistically different" compared to targeting errors at 40 seconds (0.88 mm), 60 seconds (0.65 mm), and 180 seconds (0.41 mm).
Shyn and colleagues also noted that when the SUV, or tumor-to-background, ratio was less than 1.3, targeting errors were more likely. For larger lesions and more FDG-avid lesions, there was no gain in obtaining longer than 20-second image acquisitions.
"The images may be a little bit noisier, but in terms of seeing the lesion and being able to target it, it was just as good with 20-second PET as it was with three-minute PET," Shyn said. "We think this is going to be a very useful feature as we go forward using PET/CT for guiding procedures."
The one application in which this protocol does appear to be insufficient, Shyn added, is for lesions that are minimally FDG-avid and lesions that are approximately 1 cm in size.
Previous research
This most recent study follows research by Shyn and colleagues published last year, which concluded that acquiring PET/CT datasets with respiratory bellows-assisted, monitored breath-holds improves PET/CT image registration compared to unmonitored PET/CT.
They also concluded that the technique "may facilitate accurate targeting during PET/CT-guided interventions in anatomic regions subject to respiratory motion" (Journal of Vascular and Interventional Radiology, Sept. 2011, Vol. 22:9, pp. 1287-1292).
"One of the things we noticed when we did that study was that some of these 20-second PET images looked pretty darn good," Shyn added, which prompted the most recent study and presentation at the SIR annual meeting.
"From an interventional point of view, having to wait three minutes to get a scan during a procedure seems like an eternity," Shyn said. "So, we were curious if we could get by with 20-second images. Sure enough, we can."