Breast-specific gamma imaging (BSGI) confirmed mammography, ultrasound, and MRI results in 55% of patients and identified additional malignant lesions, clarified ambiguous findings, or significantly changed patient management in 20% of cases, according to a study from California researchers.
The additional information from BSGI can help direct patients to the proper treatment and in some cases avoid unnecessary surgery, according to study co-author Dr. Marie Tartar, director of advanced breast imaging at Scripps Green Hospital in La Jolla, CA.
The study results were presented at the RSNA 2011 meeting by co-author Dr. Michelle Phillips, a hematology-oncology fellow at the University of California, San Francisco.
In an interview with AuntMinnie.com, Tartar said she is sometimes "frustrated with the limitations of anatomic imaging [and] the nonspecificity of some of the things we rely on to detect cancer, such as calcifications in a mammogram or nodules on ultrasound."
While many findings prove to be benign, there is no surefire way -- other than biopsy -- to determine which abnormalities signify cancer and which ones do not, she said.
Modality deficiencies
Scripps performs a "fair amount" of breast MRI scans, but the modality may not be suitable for patients with claustrophobia, a pacemaker or implantable device, or other MRI-related issues, Tartar said.
"In some patients, [MRI] works fantastically, but in other patients there is a lot of background enhancement, and you are sorry you even ordered an MRI," she said. "And it is well-acknowledged that mammography and ultrasound have some fairly significant limitations in terms of displaying the full extent of the disease."
Those deficiencies prompted Tartar and Phillips to initiate a retrospective study to review records, clinician notes, imaging studies, and pathology reports of 267 patients with new diagnoses of breast cancer at Scripps Clinic in 2009. Of those patients, 56 women (average age, 56.1 years) received BSGI in addition to conventional imaging prior to surgery.
The study population included 46 women (82%) with dense breast tissue on mammography. Seventeen women (30%) underwent both BSGI and MRI: BSGI was performed first in eight patients, while MRI was used first in nine patients. If the MRI results had any ambiguity, the patient then received BSGI.
Cancer was found in 58 breasts, with two patients diagnosed with bilateral cancer. The pathologic diagnoses included 18 cases of ductal carcinoma in situ (DCIS), 22 patients with invasive ductal carcinoma (IDC), 15 patients with both DCIS and IDC, and three patients with invasive lobular carcinoma.
BSGI evaluation
BSGI results agreed with conventional imaging findings in 31 (55%) of the 56 patients. BSGI identified additional malignant lesions, clarified ambiguous findings, or significantly changed patient management in 11 (20%) of the 56.
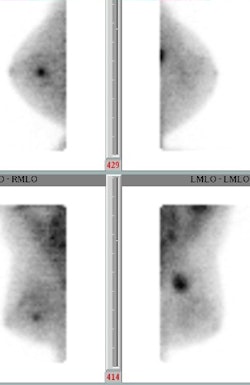 A 53-year-old woman with a new diagnosis of IDC presented with a left upper outer quadrant breast lump. BSGI clarified the extent of the lump (lower right image) and found a previously undiscovered tumor (upper left image). Image courtesy of Dr. Marie Tartar.
A 53-year-old woman with a new diagnosis of IDC presented with a left upper outer quadrant breast lump. BSGI clarified the extent of the lump (lower right image) and found a previously undiscovered tumor (upper left image). Image courtesy of Dr. Marie Tartar.In some cases, Tartar noted, BSGI showed a neoplasm that was larger than originally perceived on ultrasound, so the patient may not have been an ideal case for breast conservation, as previously thought.
Also, at times "we had unsuspected cancer in another quadrant," she said. "So, [the patient] was converted from an apparent breast conservation candidate into someone who was better served with a mastectomy."
Three patients underwent additional biopsies and five received additional imaging studies (eight of 57 cases, or 14%). Average follow-up was 426 days.
"In our experience, BSGI proves to be a cost-effective, well-tolerated, sensitive, and specific adjunct modality for enhancing presurgical planning for patients with newly diagnosed breast cancer, especially in relatively young female patients with dense breast tissue," Tartar and Phillips wrote in the study abstract.
Modality of choice
At Scripps Green Hospital, mammography and ultrasound still remain the modalities of first choice in breast imaging, followed by MRI and then BSGI as an adjunct.
"When we have a new diagnosis of breast cancer and we want to do something beyond mammography and ultrasound, our group's first choice is still MRI because we have longer experience with [MRI] and have a way to biopsy with [MRI]," Tartar said. "However, we are very happy that in patients who cannot have an MRI we have something to offer them as a reasonable alternative."
Scripps also uses BSGI in patients where a determination of breast cancer is unclear. The advantage to BSGI is that breast tissue is seen from a physiologic point of view. "In other words," Tartar said, "you are not relying on an anatomic feature, such as a calcification, that can as easily signify a benign process as it can a malignant process."
BSGI also has advantages beyond the clinical implications for patients. "It is a good thing that we have easier ways to biopsy people, but there is still a tremendous cost there -- not just an economic cost," she said. "There is a psychological cost that is not inconsiderable. I think the psychological toll on patients can be high."