The efficacy of radiotherapy is ultimately dependent upon the ability to accurately locate the target, particularly when treating organs with a tendency to move, such as the liver or prostate gland. As such, there's a real need for an imaging technique that can offer marker-free, soft-tissue visualization before -- and preferably also during -- beam delivery.
Ultrasound imaging could meet all of the above requirements, providing real-time tracking of target organ location without delivering any extra radiation dose to healthy tissue. Some of the latest work in this field was presented at the recent joint annual meeting of the American Association of Physicists in Medicine (AAPM) and the Canadian Organization of Medical Physicists (COMP) held in Vancouver, British Columbia.
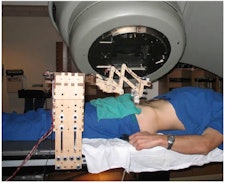 The robotic manipulator controls the pressure and position of an ultrasound transducer. The linac head can be seen behind the robotic arm.
The robotic manipulator controls the pressure and position of an ultrasound transducer. The linac head can be seen behind the robotic arm.One example is the development of a telerobotic ultrasound system for real-time detection of prostate and liver displacements, as described by Jeffrey Schlosser, a graduate student in bioengineering at Stanford University. The system uses a robotic manipulator to control the pressure and position of an ultrasound transducer on the patient and is operated via a remote interface located outside the treatment room.
Target position is monitored via continuous recording and processing of transabdominal ultrasound images, with 2D acquisition used to detect any displacements as quickly as possible. "For monitoring, we're interested in the fastest acquisition mode, which is single two-dimensional plane imaging," Schlosser explained.
During imaging, two tissue displacement parameters are extracted: the window position relative to its original position, and a coefficient of correlation with a reference image. Schlosser noted that processing time is less than 20 msec per image. The ultimate aim is to activate a beam gating signal when the displacement parameter(s) exceed a specified threshold, indicating a target shift.
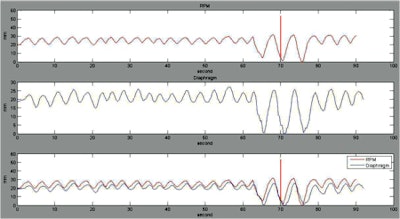
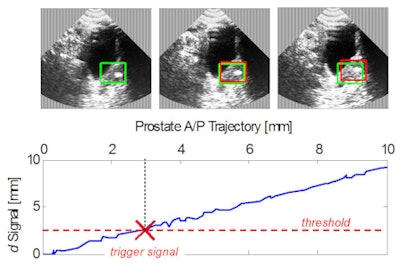 In-plane prostate displacement. The lower image demonstrates the activation of a trigger signal.
In-plane prostate displacement. The lower image demonstrates the activation of a trigger signal.The scheme was tested on a pelvic phantom and in vivo on five healthy volunteers. In the phantom, prostate translations of 1.5, 1.4, and 1.4 mm were detectable at 95% confidence in the anterior/posterior, superior/inferior, and medial/lateral directions, respectively; rotation of 1.3° was also detectable. The corresponding in vivo results were 2.3, 2.5, and 2.8 mm, and 4.7°.
With a suitable threshold selected, the rate of false positives was less than 1.5 per 10 minutes of continuous in vivo imaging. Schlosser noted that the planar tissue displacement was detected more accurately than out-of-plane displacement. "In the future, we're looking to combine this with dual-plane imaging to equalize monitoring performance in all directions," he said.
Respiratory tracking
Reliable tracking of respiratory motion can help enhance the accuracy of radiotherapy, by enabling gated delivery, for example. Ping Yan, PhD, a research scientist at Columbia University, discussed how ultrasound images of the diaphragm can be used to determine respiratory motion. She also examined the correlation between diaphragm motion and abdominal surface motion measured using the real-time position management (RPM) system.
Yan and colleagues recorded ultrasonic videos of the diaphragms of volunteers during uncontrolled breathing cycles. The ultrasound probe was held next to the RPM marker block and the two signals acquired simultaneously. An automatic tracking method was then used to extract the diaphragm motion from the ultrasound images.
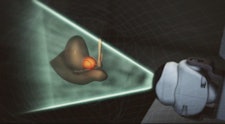
Evaluating the phase shifts between diaphragm motion and the RPM-measured respiratory signal revealed a delay of between 0.2 sec and 0.4 sec. The results also demonstrated a wide range of phase shifts between different people, as well as significant differences between different breathing cycles for the same people.
 Comparison between the RPM signal and the diaphragm motion.
Comparison between the RPM signal and the diaphragm motion.Yan concluded that ultrasound can be a more reliable method than the RPM system for respiratory gating in radiation therapy. "In [the] future, we'd like to use the respiratory signal from the ultrasound video of the diaphragm to reconstruct 4D CT images," she said. "Later, we'd like to develop an ultrasound gating system for lung radiotherapy."
Operator uncertainties
Professor Frank Verhaegen, PhD, head of physics research at the Maastro Clinic in Maastricht, the Netherlands, took a look at the Clarity system -- a 3D ultrasound system from Resonant Medical (now acquired by Elekta). Clarity is used for patient alignment in both planning and treatment rooms, enabling comparison between the two images. Reflective markers track the position of a 2D ultrasound probe, allowing volumetric images to be recorded as the probe is moved over the patient.
Verhaegen described a study looking at intra- and interoperator variability in image acquisition and matching. The study examined 13 prostate cancer patients, who received a total of 383 ultrasound scans that were used in 842 matches to reference scans. Overall, the mean intraoperator variability was 0.2, 0.0, and 0.4 mm in the x, y, and z directions, respectively, with standard deviations of 1.8, 2.2, and 2.7 mm. The mean interoperator variability was -0.2, -0.3, and -0.2 mm, with standard deviations of 2.6, 2.2, and 2.9 mm.
The researchers also examined the effect of probe pressure on prostate position. "The probe pressure effect is real," said Verhaegen. He noted, however, that as Clarity uses an intramodality approach (i.e., comparison of two ultrasound images), the prostate displacement should be the same in both scans.
Finally, the team compared ultrasound images with portal images of fiducial markers in eight patients. In the left-right direction, no correlation was seen between ultrasound and portal images. However, good (although not perfect) correlation was observed in the superior-inferior and anterior-posterior directions.
Overall, the total uncertainty of this 3D ultrasound approach to prostate localization was conservatively estimated to be 4 mm. This uncertainty is comparable to that of electronic portal imaging of fiducial markers -- the current standard for image-guided prostate radiotherapy.
Automated approach
Martin Lachaine, PhD, director of research at Elekta's Resonant Medical facility, described the development of a mechanically sweeping autoscan probe based on the Clarity system. Here, the freehand scanning is replaced with an autoscan technique, which could allow motion tracking during radiation treatment while the therapist remains in the console room.
 Automated (user-independent) scanning.
Automated (user-independent) scanning.The autoscan probe's accuracy was assessed by comparing CT and 3D ultrasound images of a phantom. Results showed submillimeter accuracy in all directions, which Lachaine noted is accurate enough for intrafraction motion tracking. Tests also demonstrated that radiation dose -- from CT scans or treatment beam -- does not affect the probe's performance.
While transabdominal ultrasound imaging is suitable for monitoring prostate position during planning or patient setup, this probe placement geometry can restrict the treatment beam direction used during radiotherapy. Thus the researchers investigated the use of transperineal ultrasound, which also benefits from a shorter skin-to-prostate distance and doesn't require bladder filling.
The first clinical study of transperineal prostate imaging has now been performed, in collaboration with researchers at the University of Vermont. The study involved 20 patients, the first 15 of whom were used to optimize image quality and patient positioning. The remaining five patients took part in a feasibility test for transperineal ultrasound imaging.
Lachaine reported that the process was well tolerated by all patients, and that the prostate and surrounding anatomy were visualized well. The next step will be to develop automated, continuous imaging for monitoring prostate motion during treatment, enabling interruption of the beam if too much motion is detected.
"The autoscan probe can be used to obtain high-quality images of prostate and surrounding soft tissue," Lachaine concluded. "Extension to 4D intrafractional prostate imaging for conventional and stereotactic body radiotherapy is feasible, and is under development."
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.