Combined stress perfusion CT imaging not only is feasible, it's potentially valuable for assessing some patients at risk of coronary artery disease in a one-modality imaging procedure, according to a study appearing this month in Radiology.
Coronary CT angiography (CTA) has proven value for detecting coronary artery stenosis, though it doesn't provide information about how a stenosis affects the heart, which is where SPECT myocardial perfusion imaging (MPI) can be useful.
But SPECT can be replaced with CT perfusion imaging, which has revealed comparable strength in detecting clinically significant stenoses, accurately assessing infarct size and myocardial viability. Studies have also shown the value of combining coronary anatomy and myocardial perfusion assessment for detecting obstructive coronary artery disease.
What researchers from Massachusetts General Hospital in Boston wanted to know was how well their particular CT perfusion protocol worked, and whether the perfusion results offered important information beyond what was already provided by dual-source coronary CT angiography for detecting coronary artery disease in a high-risk population.
"We found CT perfusion to have incremental value at cardiac CT angiography for the detection of hemodynamically significant [coronary artery disease]," wrote Dr. Jose Rocha-Filho and colleagues in Radiology (February 2010, Vol. 254:2, pp. 410-419).
The group enrolled 35 patients (mean age, 61.2 years ± 10.7), all of whom were at high risk for coronary artery disease. Eighty-three percent were men, 43% were obese, 66% were current or former smokers, and 63% had experienced angina pectoris, including 37% with a previous myocardial infarction.
Following administration of 10 mL contrast at 4 mL/sec (Isovue 370, Bracco Diagnostics, Princeton, NJ) and a saline flush, all patients underwent retrospective electrocardiogram (ECG)-gated adenosine stress perfusion CT followed by prospective ECG-gated rest CT perfusion imaging (2 x 32 x 0.6 mm, 100-120 kV, 330-370 mAs) on a dual-source CT scanner (Somatom Definition, Siemens Healthcare, Malvern, PA). Images were reconstructed using 0.75-mm slice thickness at 0.4-mm increments at every 10% of the cardiac cycle.
Three experienced readers evaluated all of the data independently, unaware of the clinical results, Rocha-Filho and colleagues wrote. Once the stenoses were analyzed for severity, the myocardial perfusion defects at CT perfusion were scored for severity and reversibility. Finally, coronary artery stenosis was reclassified according to perfusion findings at the combined exams.
The results showed improvement in all measures of diagnostic accuracy after consideration of the CT perfusion images.
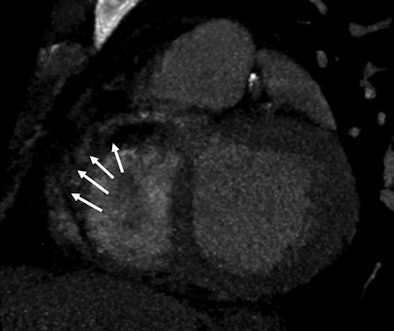 |
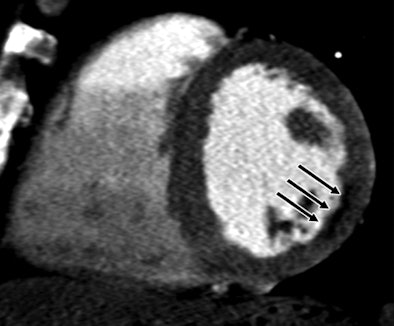
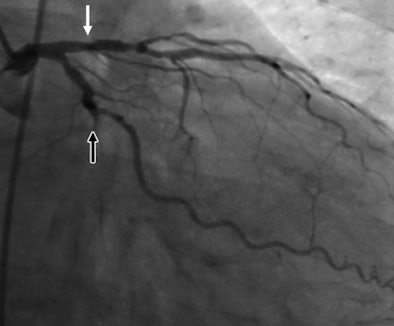
| A 51-year-old man with history of diabetes mellitus presented with typical angina. Above, curved multiplanar reformatted cardiac CT angiographic image read before perfusion shows prominent motion artifact in right coronary artery (arrows) that persisted through all cardiac phases. Below, thick short-axis CT perfusion image at midventricular level shows perfusion defect (arrows) during stress CT perfusion in the inferior and inferolateral segments that is partially reversible during rest CT perfusion. Bottom, reference-standard invasive angiogram findings confirm the presence of severely stenotic lesion in right coronary artery (arrow) that was seen at postperfusion cardiac CTA image reading. Images republished with permission of the Radiological Society of North America. |
 |
 |
With a threshold of greater than 50% luminal narrowing used to define stenosis, the stenosis severity for 26 (25%) of the 105 vessels analyzed was reclassified, and the stenosis severity for 79 (75%) vessels was not, Rocha-Filho and colleagues wrote.
Moreover, the stenosis severity of 64 (81%) of the 79 vessels that were not reclassified was "ultimately in agreement" with that rendered by quantitative coronary angiography performed in all patients as the reference standard, they wrote.
|
|||||||||||||||
| PPV = positive predictive value; NPV = negative predictive value. |
The results above show that at the 50% luminal narrowing threshold for significant stenosis, stenosis detection improved significantly after the initial (preperfusion) findings at coronary CTA when compared with the results from CT perfusion. With the final perfusion analysis findings, the area under the receiver operator characteristics (ROC) curve increased significantly from 77% to 90% (p < 0.005).
"We found that the combination of cardiac CT angiography and CT perfusion imaging in a single examination was feasible and facilitated improved diagnostic accuracy, a higher level of reader confidence, and better interobserver variability," the authors wrote.
The combined protocol of adenosine perfusion CT imaging and cardiac CTA adds incremental value to cardiac CT angiography in detecting significant coronary artery disease, they added.
"Such a protocol may be particularly valuable in the examination of patients with a high pretest probability of CAD, since they are usually found at presentation to have a large calcific plaque burden that leads to lower overall image quality and diagnostic accuracy," Rocha-Filho and his team wrote.
A previous study using 64-detector-row CT revealed that in patients with a high pretest probability of disease, coronary CT angiography alone may miss as many as 17% of patients, they added. These patients are generally referred for myocardial perfusion imaging and/or invasive angiography -- and some of these tests could be replaced by the new protocol.
As for limitations, the authors cautioned that their protocol requires double the contrast dose needed for conventional CT angiography and should be avoided in patients with renal dysfunction. In addition, prospectively triggered axial scans were not used for the stress perfusion studies. Although this approach would have lowered the radiation dose, the "chronotropic effects of adenosine" would have increased heart rates beyond what is optimal for CT scanning, the authors stated, noting that improving scanner technology is expected to boost image quality further.
By Eric Barnes
AuntMinnie.com staff writer
February 9, 2010
Related Reading
DECT cuts tests as a one-stop myocardial, coronary artery exam, August 10, 2009
Adenosine stress DECT equivalent to SPECT, MRI, November 21, 2008
Dual-source CT edges into cardiac SPECT turf, March 6, 2008
Study correlates CTA to angiography, myocardial perfusion SPECT, May 25, 2007
Stress MPI with Tc-99m SPECT identifies high-risk obese patients, September 1, 2006
Copyright © 2010 AuntMinnie.com