Radiation dose delivered to obese patients during radiography and fluoroscopy procedures may be higher than previously estimated -- and could be reaching levels as high as 28 mSv for an abdominal x-ray exam, according to a new study. But careful patient positioning may be able to help reduce dose in the obese.
In a study published online April 29 in Radiology, lead researcher Jacquelyn Yanch, Ph.D., of Massachusetts Institute of Technology in Cambridge, MA, looked at radiation dose delivered during radiography and fluoroscopy procedures. The purpose of the study was to estimate the increase in effective radiation dose from diagnostic x-rays for overweight and obese adult patients, and to determine whether existing dose reference levels are accurate.
"Our study showed that a little bit of fat doesn't make too big of a difference, but since x-rays are stopped exponentially with increasing thickness, when you have several centimeters, your dosage goes way up," Yanch said.
Fat's impact on dose
Fat can have an attenuating effect on x-ray beams, and equipment operators are often forced to turn x-ray output up to achieve acceptable images. But estimates of the amount of radiation dose that obese patients are receiving might be too low, because existing dose estimates are based on Reference Man, a reference individual that was developed in the early 1970s based on data from the first part of the 20th century.
Reference Man was meant to represent the typical 20- or 30-year-old male from North America and northern Europe, but due to rising obesity levels, these anatomic characteristics no longer accurately reflect the general U.S. population, the study authors noted.
"He probably did adequately represent the male adult population back then, but he certainly doesn't now," Yanch said.
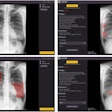
To more accurately measure how much dose existing patients are getting, the investigators developed a computer simulation of what Reference Man -- as well as Reference Woman -- might look like today.
"We added fat under the skin of the phantoms in different proportions, front, sides, and back," Yanch explained. "We calculated dose again and looked at how much the dose went up as a function of not just the thickness of fat, but the distribution around the body."
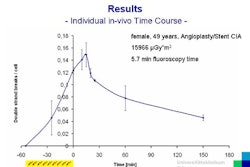
The differences were dramatic. For example, a typical abdominal radiographic examination for a lean person delivers an effective radiation dose of approximately 0.70 mSv, according to the authors. But with 25 cm of additional fat, a patient's dose could increase by a factor of 20 or more, leading to a dose per exam of up to 28 mSv.
At this level, the radiation dose from four abdominal radiographs would exceed 100 mSv, which, according to existing linear no-threshold models for calculating cancer risk, would result in a one in 170 chance of the patient developing cancer from the imaging study, the authors wrote.
Even that estimate is uncertain, however. The linear no-threshold model is based on relatively small numbers of atomic bomb survivors receiving doses in the same range under extremely different conditions.
"We just don't know enough about radiation-induced cancer in this dose range," Yanch said.
Patient positioning
On the positive side, the study showed that exponential radiation dose increases can be avoided through careful patient positioning. For fluoroscopy and conventional radiography, the patient's orientation in the beam and where the largest thickness of fat lies do matter.
"You can change a patient's dose for a reasonably large patient by a factor of three or four simply by turning him over, depending on what body type he has and where the thickest amount of fat is," Yanch explained. "You can orient that closest to the beam ... giving the patient a significant dose sparing."
Yanch hopes that the research will emphasize the importance for radiology professionals to be conscious of the magnitude of radiation dose in the obese, and to incorporate that into their decision-making process. In addition, she stressed the importance of incorporating patient exam history into prescribing radiological studies, as well as the importance of developing more accurate models than A-bomb survival data for predicting the relationship between dose and risk.
Moving forward, either a change to Reference Man has to occur, or a new strategy for monitoring an individual's dose must emerge, according to Yanch.
"We shouldn't just assume body size and shape, and that anyone who gets that particular exam gets that particular dose," Yanch explained.
Currently, Yanch is looking at CT and how body fat affects that modality, with a particular focus on pediatric phantoms. Preliminary data show significant increases in dose in CT, as well, she said.
By Lin Muschlitz
AuntMinnie.com contributing writer
May 19, 2009
Related Reading
Computer-assisted ultrasound aids liver imaging in obese children, May 8, 2009
Obesity, diabetes interfere with ultrasound detection of fetal anomalies, April 23, 2009
When zoos refuse: Obese patients face shortage of large-capacity scanners, September 24, 2008
Rampant U.S. obesity strains imaging devices, November 28, 2007
Obesity forces radiology to supersize, enhance x-ray technology, March 1, 2007
Copyright © 2009 AuntMinnie.com