Scheduling radiation therapy sessions to occur in the morning can reduce side effects for patients with head and neck cancers, according to a Canadian study published in the International Journal of Radiation Oncology, Biology, Physics.
|
Time spent on mucositis treatment The incidence of radiation-induced mucositis is increasing with the use of intensive radiation fractionation and concurrent chemotherapy treatment for head and neck cancer patients. Mucositis can cause inability to tolerate food and/or fluids, leading to weight loss, dehydration, and feeding tube dependency. Management of a patient with mucositis typically requires more time invested by radiation oncologists, therapists, and nurses than with many other types of patients receiving radiation therapy treatment. The results of a Web-based survey evaluating the burden of mucositis management on radiation therapy staff was presented as a poster at the 2008 annual meeting of the American Society for Radiation Oncology (ASTRO) last fall. Fifty radiation oncologists and 51 registered oncology nurses responded to a questionnaire sent to 1,200 randomly selected members of ASTRO and the Oncology Nursing Society (ONS) in October 2007. Respondents were required to be treating at least three patients with head and neck cancers per month. Physicians reported that they spent 7.2 hours of unreimbursed time per patient managing mucositis-related activities, from planning to post-treatment, and nurses spent 12.1 hours. During the treatment time, physicians reported that the average time spent per patient increased each week from 30 minutes for week 1 to 1.4 hours by week 7 of treatment. Nurses spent an average of two hours by week 7. Assuming treatment of 60 patients per year, researchers from Covance Market Access Services of Gaithersburg, MD, estimated that physicians would spend 431 hours of unreimbursed time and nurses would spend 871 hours. The survey was underwritten by Amgen of Thousand Oaks, CA. |
But a long-term clinical trial conducted at 12 Canadian cancer centers has determined that the time of day that treatment is given makes a difference for patients receiving 66-70 Gy of radiation in 33 to 35 fractions. Patients treated with this protocol of radiation therapy with morning appointments stopped losing weight sooner than patients with afternoon appointments. Morning appointments were also more beneficial for patients who did not stop smoking during the treatment time period.
The study, published in the January 2009 issue of International Journal of Radiation Oncology, Biology, Physics (Vol. 73:1, pp. 166-172), was conducted to determine if circadian rhythm in cell cycle progression of gastrointestinal mucosa affected the extent of toxicity caused by radiation therapy treatments. In August 1999, at the outset of the clinical trial, researchers hypothesized that radiation therapy delivered during the morning would be associated with less oral mucosity.
But time of day did not prove to be statistically significant in reducing mucositis toxicity, according to principal investigator Dr. Georg Bjarnason, a radiation oncologist at Sunnybrook Odette Cancer Centre in Toronto.
For the clinical trial, cancer centers from Newfoundland to British Columbia enrolled a total of 216 patients with squamous cell carcinoma of the oral cavity, pharynx, or larynx. All had two or more directly visible areas of mucosa greater than or equal to 6 cm2 in size, did not have abnormal sleep habits, did not work evening or night shifts, and had not received previous radiation therapy treatments.
The patients were enrolled in the clinical trial between August 1, 1999, and November 15, 2004, to be equally divided between morning and afternoon treatments. Eleven patients were disqualified for various reasons during the trial.
The 85 men and 49 women remaining had a median age of 60 years. The 60 smokers were evenly divided between the two groups (26.9% versus 24.5%), as were patients who drank alcohol (42.3% versus 41.2%) during therapy. The patients who completed radiation therapy were stratified into four target dose groups, which are shown in the following table.
The patients in each target group were randomized to receive a daily fraction of radiation therapy either between 8:00 a.m. and 10:00 a.m. or 4:00 p.m. and 6:00 p.m. on weekdays.
|
Prior to treatment and on a weekly basis thereafter during the treatment period, patients were weighed, questioned about use of tobacco and alcohol, evaluated based on Eastern Cooperative Oncology Group (ECOG) performance status, assessed for level of mucositis using the Radiation Therapy Oncology Group (RTOG) mucositis score as well as a second previously validated scoring system, and were given a quality of life (QOL) score using a head and neck radiation therapy questionnaire evaluating six domains (oral, skin, throat, energy level, psychosocial behavior, and digestive).
Patients were then evaluated on a weekly basis until mucositis had peaked, and subsequently every two weeks after that until mucositis was classified as less than grade 2. Both a mucositis scoring system and the QOL head and neck radiation therapy questionnaire were used.
At every subsequent follow-up visit during a 24-week period following therapy, patients were administered the QOL head and neck radiation therapy questionnaire. All patients were weighed, evaluated based on ECOG performance status, and assessed for toxicity other than mucositis at two to three, six to eight, 12, and 24 weeks after the last radiation dose and followed for survival for a period of three years.
Prior to clinical trial implementation, the researchers had hypothesized that based on a sample of 216 patients, 17.5% of the morning group and 35% of the afternoon group would develop oral mucositis at grade 3 or greater. Instead, 52.9% of the morning group and 62.4% of the afternoon group had at least one episode of RTOG grade 3 mucositis. This was not statistically significant due to the sample size. No significant differences were reported between the two groups with respect to the interval between initial treatment and development of mucositis to grade 2 and greater or in its length of duration.
However, morning treatments produced much better results for patients receiving 66 Gy in 33 fractions or 70 Gy in 35 fractions. To summarize:
|
Smokers in all groups benefited from morning treatments, with only 42.9% of the total developing grade 3 or greater mucositis, compared with 76% who received afternoon treatments.
Morning treatments offered one other advantage -- although all patients lost similar amounts of weight in the first five months, patients with morning appointments on average stopped losing weight at that point. Patients receiving afternoon treatments continued to lose weight for an additional four months, on average.
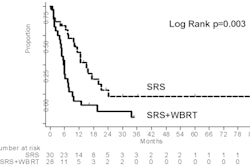
The difference in two-year survival rate was statistically insignificant, at 61.1% for the morning group and 64.1% for the afternoon group. A total of 71 patients died during the study period, 37 in the morning group and 34 in the afternoon group.
By Cynthia E. Keen
AuntMinnie.com staff writer
February 26, 2009
Related Reading
Sequential and alternating chemoradiotherapy comparable for laryngeal cancer, February 6, 2009
Aspiration widespread in head and neck cancer patients, January 9, 2008
Copyright © 2009 AuntMinnie.com