FDG-PET is showing early promise in the accurate detection of infected knee prostheses, but researchers caution that more patient samples are needed to verify the imaging technique's efficacy.
The diagnosis of infection in knee prosthesis is key to successful implementation. "There could be some obvious signs, such as inflammation, but sometimes the prosthesis structures are difficult to evaluate," said Dr. Abass Alavi, study co-author and chief of the nuclear medicine division at the University of Pennsylvania Medical Center in Philadelphia. "While some patients' conditions can be corrected by replacing one prosthesis with another, if there is infection that can be detected beforehand, we can completely change the way we manage these patients."
Patients can be treated with an antibiotic after the prosthesis is removed, proceed to treatment for the infection for six weeks to six months, and then have a prosthesis implanted again.
"As we started using FDG-PET for oncology, we realized that FDG is not only picked up in cancer cells, but also in inflammatory tissues," added Alavi in his presentation at the 2008 SNM meeting in New Orleans.
Infection risk
Alavi believes that FDG-PET may be much more effective in infection detection than other tests used more commonly today. Clinical pathological tests, such as aspiration, for example, are prone to error and "any time you aspirate these joints, there is a possibility and probability, in fact, that you will introduce bacteria to the unaffected joint," he said.
In the retrospective study, based at the University of Pennsylvania Medical Center and Thomas Jefferson University in Philadelphia and funded by the National Institutes of Health (NIH), FDG-PET was performed on the affected knees in 52 patients with a painful prosthesis after clinical evaluation and laboratory data were inconclusive for infection.
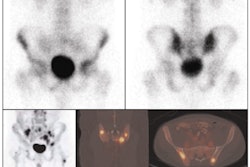
PET scans were performed 60 minutes after injection of FDG. Final clinical outcome was available for 31 patients (36 knees) of 52 enrolled in the study, with clinical diagnosis based on surgical assessment, microbiology results, and follow-up studies.
Images were interpreted in blinded fashion, with infection identified based on increased FDG uptake at the bone-prosthesis interface versus adjacent tissue. Images then underwent a second blinded read by a single senior nuclear medicine radiologist to eliminate interobserver variability.
Sensitivity/specificity
Upon further analysis, researchers found that FDG-PET correctly identified infection in six of seven cases for a sensitivity rate of 86%. There were false-positive results in two of 29 prostheses for a specificity of 93%. Positive predictive value was 75% (six of eight cases), negative predictive value was 96% (27 of 28), and accuracy was 92% (33 of 36), as interpreted by staff radiologists.
In the second blinded read, sensitivity remained at 86% (six of seven cases), while specificity increased to 100% (29 of 29). Positive predictive value also increased to 100% (six of six), negative predictive value rose to 97% (29 of 30), and accuracy improved to 97% (35 of 36).
Alavi noted that the high rate of specificity "is very important in this population, because having a higher specificity allows us to send these patients to an outpatient group with no difficulty."
He described the 86% sensitivity rate as "pretty good" but added that more research must be done to determine the reliability of that percentage. "We have to have a larger sample of patients to see how it holds," he said.
The collection of more patient data may prove to be a big hurdle for researchers. Currently, there are few healthcare facilities in the U.S. that use FDG-PET to detect infection, and there is no reimbursement on the immediate horizon from the Centers for Medicare and Medicaid Services (CMS).
Reimbursement rebuke
This past March CMS declined to extend Medicare coverage for the use of PET for several infection and inflammation indications, ruling that there is not enough evidence to conclude that FDG-PET for chronic osteomyelitis, infection of hip arthroplasty, and fever of unknown origin improves health outcomes.
The CMS review for coverage of PET applications in inflammation and infection was prompted at the request of Alavi in June 2007.
During his presentation at the SNM meeting, Alavi said the only comments to CMS came from his own students at the University of Pennsylvania. "We tried to see how we can best prove [FDG-PET] to be effective, but the options are very limited," he said. "It's a catch-22 because so few facilities use the technique, so there is not enough experience to get samples" of FDG-PET's efficacy.
He hoped that the NIH would fund clinical trials in this area "because it is such a big healthcare issue" for prosthesis and for infection in general. "If we had FDG-PET for the detection of inflammation, it would be as big as cancer, and we can do much, much more for infection patients than we can do for cancer patients," Alavi said. "It is unfortunate that it takes so long for something that works so well to be allowed to be used routinely."
By Wayne Forrest
AuntMinnie.com staff writer
August 18, 2008
Related Reading
SNM's Images of the Year show molecular imaging's head-to-toe prowess, June 16, 2008
CMS declines PET coverage for infection, inflammation, March 20, 2008
FDG-PET successfully diagnoses chronic osteomyelitis, July 21, 2006
PET update on skeletal applications highlights infection, osseous metastases, October 7, 2003
Infecton SPECT, FDG-PET illuminate skeletal infections, June 20, 2002
Copyright © 2008 AuntMinnie.com