According to the U.S. Centers for Disease Control and Prevention (CDC), breast cancer is the second most common form of cancer in all women (after nonmelanoma skin cancer), and is a main cause of cancer death among certain ethnic groups, such as Hispanic and African-American women.
Then there is another subset of women whose family health history and genetic makeup puts them at an even greater risk. In March 2007, an expert panel at the American Cancer Society (ACS) recommended that women who meet the following criteria should undergo MR imaging along with mammography:
- Women who are BRCA-1 or BRCA-2 mutation carriers
- Women with a first-degree relative who are BRCA mutation carriers, but who have not undergone genetic testing themselves
- A lifetime risk of breast cancer of at least 20% to 25% using standard risk assessment models (BRCAPRO, Claus, and Tyrer-Cuzick)
- Prior radiation treatment to the chest between ages 10 and 30 for other reasons such as Hodgkin's disease
- A first-degree relative who carries a genetic mutation in the TP53 or PTEN genes (Li-Fraumeni syndrome and Cowden and Bannayan-Riley-Ruvalcaba syndromes)
In anticipation of an increased need for breast MR services, many radiologists are considering implementing the modality in the inpatient and outpatient setting. This article tackles some of the issues that breast centers will face as they integrate breast MR into their practice, and offers advice from breast MR experts on how to make that transition as smooth as possible.
Personnel
Implementing a proper breast MR program will most likely mean more hiring. For example, the role of the nurse in MRI has gone beyond assisting with sedation to include patient advocacy.
For many patients, a cancer diagnosis throws them into an emotional, physical, and social whirlwind. Proceeding through a course of care could be a very daunting task, so a nurse can act as a liaison between the patient and healthcare team. Dr. Harold Freeman of Harlem Hospital in New York City developed this concept of a patient navigator nearly 30 years ago. A nurse navigator can provide individualized support, including appointment facilitation, communication with physicians, and support during treatment and recovery, and act as a single source for education as well as advocacy.
Of course, hiring new staff may not be practical for a start-up breast health center. But new breast centers can take advantage of the efforts of national and local breast cancer advocacy groups, most of which offer excellent patient education material that they are willing to share.
MR technologists
On the technical side, technologists who perform breast MRI must be sensitive to the needs of their patients and possess excellent communication skills. These patients may have anxiety that requires particular reassurance. The technologist may be called upon to reiterate the information that the patient first received from the nurse navigator.
If a technologist can keep the patient comfortable and informed, it can reduce the likelihood of motion-induced artifacts and repeat sequences. Technologists with prior mammography experience are well-suited to perform breast MRI and image-guided biopsies.
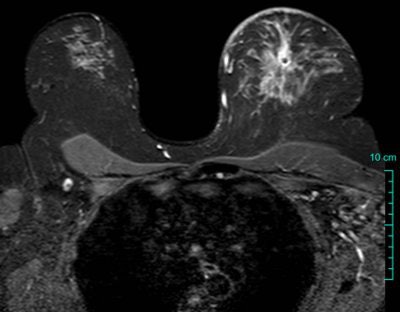
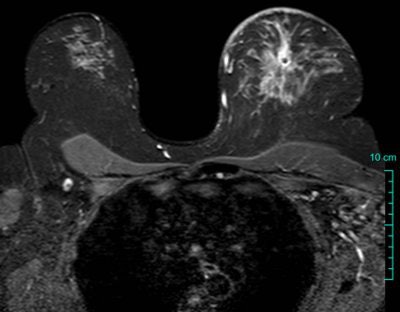 |
| To maintain consistency in breast MRI, it's important to position patients properly and instruct them to remain still. A little communication goes a long way toward ensuring image quality. Proper protocol selection allows visualization of breast parenchyma, skin, axillae, and other structures as seen on this axial T2-weighted image. Image courtesy of Dr. Mark Lawton, Wheaton Franciscan Healthcare, Milwaukee. |
Breast MR technologists should have a firm grasp of MR physics, breast pathophysiology, and mammography, according to Dr. Gary Whitman, an associate professor of diagnostic radiology at M. D. Anderson Cancer Center in Houston. They should also understand how to effectively position the breast tissue in the MRI coil for optimal image quality.
Dr. Kathy Schilling of Boca Raton Community Hospital in Florida said she looks for a technologist who is detail-oriented. "Every exam needs the female patient to be positioned appropriately and must be performed in a consistent fashion. This gives the radiologist the ability to interpret the exam consistently. Only a subset of technologists perform breast MRI in our center as well as biopsy," said Schilling, who is the director of breast imaging at the hospital's Women's Center.
Finding the right technologist isn't as easy as simply cross-training a mammography technologist in MRI or vice versa. The American Registry of Radiologic Technologists (ARRT) offers advanced examination in mammography and MRI. Ideally, the MR technologist should possess credentials in both.
Alternatively, creating a cooperative team of mammographers, stereotactic technologists, and MRI technologists can be a successful approach as each team member offers his or her expertise. Above all, patient safety should be a primary focus of training for technologists and ancillary staff working in the breast MR environment.
A multimodality, multidisciplinary approach
Imaging economics consultant Christine Hughes of Chicago-based Hadley Hart Group was involved in launching some of the first mobile MRI systems in the U.S. In her opinion, the adoption of breast MRI by mainstream medical imagers will be influenced by how much training radiologists receive.
Hughes cited the Boca Raton facility as a prime example of an all-in-one place that provides patients with continuity of care. Patients have easy access to screening, diagnostic services, and oncology or surgical specialists. An onsite geneticist is available for testing and counseling. The facility offers mammography, ultrasound, breast MRI, and breast biopsy in an outpatient setting.
"We work closely with our referring physicians, in particular the surgeons. We do not want to delay surgery, so we actively schedule patients for additional imaging and biopsy generated as a result of MRI," Schilling said.
This approach is also taken at AnMed Health in Anderson, SC, where the breast imaging department (including MR) is located in the same building as surgery and oncology. Additionally, a dedicated breast cancer tumor board weekly reviews cases -- from diagnosis to pathology -- with radiologists, pathologists, surgeons, oncologists, and radiation therapists in attendance, said Dr. Paige Huber, chief of breast imaging at AnMed.
Hughes stressed that being multidisciplinary in name only is not enough: There needs to be easy access to all specialties, not only for the patients but for physicians as well. Radiologists should meet regularly with primary care physicians, ob/gyns, surgeons, and oncologists to formulate approaches that will best serve their common patients. In turn, this doctor-to-doctor pathway should be clearly communicated to patients -- another instance in which a nurse navigator can be of tremendous assistance, she added.
"Breast imaging centers need to make a commitment to more than just a pink mammography room," Hughes said. "The handoff of a patient between medical specialists is important."
Billing and reimbursement
Reimbursement for any medical service depends upon various factors, including geography, negotiated contract rates, and whether the services were provided on an inpatient or outpatient basis. Billing department personnel should be well-versed in reimbursement policies, appropriateness criteria, and payor plans. This information should be clearly communicated to patients to set expectations appropriately.
Additionally, it's important to educate the referring community along with the payors during any implementation of new technologies and apply the correct CPT and ICD-9 codes to ensure reimbursement.
There is no getting around the fact that reimbursement for breast imaging is low. The reality is that only those centers with high-volume mammography screening rates are in a position to start adding other modalities to their services, Schilling said, adding that she believes that regional comprehensive breast centers will be the model of the future because of the higher volume and ability to provide greater resources.
In the meantime, an attitude adjustment as to breast MRI's value needs to occur. Recommendations such as those made by the ACS can bolster breast MR's case, as will ongoing clinical studies.
"The economic cost of breast MRI is an issue," Huber said. "However, so is all MRI.… If a patient is having knee pain and it is interfering with their golf game, no one hesitates to order a knee MRI. So why is spending money for a breast MRI on a patient with breast cancer any different?"
By Bernadette M. Kaufman, R.T.
AuntMinnie.com contributing writer
November 2, 2007
Bernadette Kaufman, a registered MR technologist, is the manager of educational initiatives and partnerships at Invivo of Orlando, FL. Having worked in diagnostic imaging for two decades and across multiple modalities, Kaufman has served on education committees for the American Society of Radiologic Technologists (ASRT) and the Society of Magnetic Resonance Technologists (SMRT). She is a regular contributor to scholarly journals and textbooks on diagnostic imaging.
The opinions expressed in this article are those of the author, and do not necessarily reflect the views of AuntMinnie.com or Invivo.
Related Reading
MRI beats US for breast screening of at-risk women, but yields more biopsies, August 6, 2007
Breast MRI helps guide surgical treatment, May 22, 2007
MRI becoming more efficient in breast cancer detection, May 18, 2007
Mammography still offers advantages over breast MR in DCIS, April 20, 2007
MRI useful for detecting cancer in contralateral breast, March 28, 2007
Copyright © 2007 AuntMinnie.com



















