As MRI magnets get stronger and active shielding compresses magnetic fields further, the distance between a gentle tug and a life-and-death tug-of-war is reduced to mere inches. MR staff and patients are often lulled into a false sense of security, thinking that objects are safe in the magnet room because they feel no immediate attraction. However, just a step or two closer and they've entered that portion of the magnetic field where the strength increases exponentially and ferromagnetic objects can become lethal missiles.
Some facilities try to exploit this rapid increase in attractive force by using conventional medical equipment in the MRI room and keeping the devices outside the area of the greatest attraction. These seat-of-the-pants protocols (e.g., it's safe as long as it's at the end of the patient table) open the door to mishaps and accidents that are completely avoidable with the use of proper equipment.
There's also the issue of mechanical and electronic equipment's function when enveloped by magnetic fields. Are you sure that the med pump -- which has to stay tethered to the wall to keep from flying across the room -- is actually delivering the prescribed dose of medication to the patient? How might the magnetic field be altering the programmed function from what was intended?
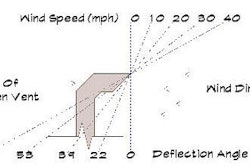
Even some pieces of medical equipment designed for use in the MRI suite come with instructions on the maximum magnetic field exposure. Some ventilators and anesthesia machines, for example, are identified as safe up to a maximum magnetic field exposure. If that threshold is 300 gauss, do you know where the field reaches this strength near your magnet? The size and shape of the 300-gauss limits are going to be different for each magnet strength and format, so there are no viable rules of thumb.
Many have recommended physical demarcation of the 5-gauss exclusion zone around an MRI so that areas of potential biostimulation hazard are plainly visible. Facilities using medical equipment that has manufacturer conditions for maximum magnetic field exposure should also consider indications on magnet room floors or walls to indicate the safe thresholds for equipment use.
But if 300 gauss is the critical value, how do you find the location of that field strength when most vendor's templates stop at 100 gauss or less?
You can either attempt to measure the field strength yourself with a gaussometer (which may be both complicated and dangerous) or you will need to contact the magnet vendor to get from them the isogauss mappings. It may require a little diligence to get to the person who can answer questions about system performance that aren't on the most commonly referenced documents.
The other potential condition for some equipment intended for use in the magnet room is that of maximum spatial gradient. Spatial gradient is the rate at which magnetic field strength increases as you move through it. If you had a plan of a magnet that showed every single gauss line, the spatial gradient would be a measurement of how close together those lines would be (or how many gauss of increase over a given distance).
Spatial gradient has a more direct impact on attractive forces than even magnet strength. These attractive forces can have impacts on mechanical equipment; however, MRI system vendors are often unable or unwilling to share information on spatial gradient, its maximum values, and physical locations. In these instances, you are well advised to contact the vendor of the ventilator or other device to get its guidance for use of its product with your magnet system.
With the proliferation of medical and ancillary equipment specifically designed for use in the MRI suite, it is inconceivable that healthcare providers would jeopardize the safety of their patients with inappropriate devices. Imaging providers should carefully evaluate the clinical needs of their patients and determine the equipment that is needed to serve them best. These choices may have implications for magnet room layout and design, but every effort should be made to ensure that equipment is used in accordance with the manufacturer's conditions for use.
The physical design of your MRI suite, including markings for patient safety and equipment operation, should be directly aligned with the care you provide. Evaluate suite design against your best practices every time you change MRI or incidental equipment, clinical applications, or operational protocols. Small changes in your layout, design, or finishes may help you further enhance the quality of care you deliver to your patients.
By Tobias GilkAuntMinnie.com contributing writer
December 29, 2006
Reprinted from http://www.mri-planning.com/ by permission of the authors. If you would like more information on any aspect of MR facility design or safety, please contact Robert Junk or Tobias Gilk at Jünk Architects.
Related Reading
Converting to new 'MR Safe' is hardly a fly-by-night effort, November 22, 2006
I see dead magnets -- could your quench pipe be a killer? November 16, 2006
MRI accident data: You don't know more than you think you do, October 27, 2006
DRA and MR patient throughput -- reimbursement cuts vs. unconventional wisdom, October 17, 2006
Burying an MRI: A tragedy in two acts, September 25, 2006
Copyright © 2006 Jünk Architects, PC