The Hospital for Special Surgery (HSS) was founded in 1863 in New York City and is the oldest existing orthopedic hospital in the U.S. The 142-bed facility performs more than 17,000 orthopedic surgery procedures a year, and has achieved a number of milestones, including the first total knee replacement, new MRI protocols for evaluating cartilage, and minimally invasive spine surgery techniques that eliminate the need for spine fusion.
Dr. Helene Pavlov is radiologist-in-chief of the hospital's radiology department. She has been a board-certified radiologist since 1976, and has published more than 100 investigative original research articles, 62 book chapters and review articles, and is first author on three textbooks. In the interview below, she talks with AuntMinnie.com about the unique challenges facing medical imaging in the orthopedic environment, and about the technologies that will change the discipline in the future.
 |
| Dr. Helene Pavlov, radiologist-in-chief of the Hospital for Special Surgery. |
AuntMinnie: Can you tell us about the Hospital for Special Surgery?
Pavlov: HSS is affiliated with the Weill Medical College of Cornell University and our academic appointments are from there. We are affiliated with New York-Presbyterian Hospital, primarily for orthopedics.
Our mission is to provide the best musculoskeletal imaging that is possible, to constantly be advancing the field. One of the benefits that we have is that we are focused on orthopedics and rheumatology, and all our modalities are geared to the musculoskeletal system. We can report on pathology faster because we see more of it daily. It's not like there's time devoted to GIs and GUs and other body parts on our imaging equipment.
All of my faculty are musculoskeletal fellowship-trained, or have extensive experience in musculoskeletal work, which allows us to be on the cutting edge of what we do.
How many images do you do a year in the department?
We do approximately 180,000 imaging exams yearly, all musculoskeletal. We have currently five MRs: one ... 0.7-tesla, one 3-tesla, and the other three are 1.5-tesla units. We also have a 16-slice CT scanner, four ultrasound rooms dedicated to musculoskeletal imaging with extended field-of-view capabilities, and we are doing research in all of those areas.
We have just recently converted from analog to CR/DR, and to be very honest have found a lot of issues with trying to do extremity work, which required dedicated applications that we identified and implemented. I think our quality on digital imaging is superb.
This is my own editorial comment, but most of the CR/DR systems appear to be set for chest and abdomen, whereas our work is geared to bones, the skeleton, spine, and extremities. Extremity work requires fine detail, because we are looking at very small changes to try to detect abnormalities as early as possible. We're not waiting for them to be so blatant that anyone could diagnose them, but we are trying to be on the cutting edge in diagnosing them as early as possible.
How unique is the hospital in its focus on musculoskeletal imaging? Are there many other hospitals out there like you?
I believe that we are very unique. In Europe, they are looking to us in developing similar orthopedic hospital models based on the way we do things here.
From a fellowship perspective, very few hospitals are dedicated specifically to orthopedic conditions and run an academic program.
Why do you think that is?
I haven't a clue. Orthopedics is tough in that you will probably find a lot of imaging sites connected with orthopedic practices. Orthopedic surgeons in general are very aggressive and want to take control, so they set up their own practices, with their own MRs and their own CTs. I know there is a lot of controversy about this, but that is out there.
How do you feel about the trend in which orthopedic physicians are purchasing equipment to operate in their own offices?
I feel very, very strongly that imaging should be done on a consultant basis and should not be done by people who benefit by finding a finding. Radiologists are supposed to be consultants to other physicians, that's what I went into radiology for. I don't want to get paid more if I find a finding requiring intervention or additional imaging studies if the study is normal.
There is an inherent bias if you are going to benefit by finding something, or even finding something that is going to require you to take a knife and do something to see if it's real. I think patients are naïve to this.
We (radiologists) go for four years (of education) during residency, and for fellowship afterward ... we are specialists. That should not be undervalued to the extent that it is, that a nonradiologist feels that they know more than we do.
I feel very strongly that all imaging is not created equal. Imaging, like the computer industry, is changing daily. From a patient's perspective you want to be able to get the state of the art at all times, both in the acquisition of the images with the technology and in the interpretation of it. It's hard for small private practices to be able to do that just from a financial perspective, as hospitals are able to do.
Can you share with me how you operate the radiology department, and how you handle training and other issues to make sure your staff is up to speed on the latest musculoskeletal imaging techniques? Are there operational differences in terms of how you run things compared to a more general hospital?
We are very research-focused. We are trying to stay on top of the research field and in some instances lead it.
For instance, in MRI, because we are an orthopedic hospital, we saw there was a need to image around metal hardware. Initially it was felt you couldn't do that, the images weren't great. We have been able to overcome that, because most of our patients have metal in them, by changing pulse sequences, coils, etc., and having skilled radiologists, under the direction of the division chief Dr. Hollis Potter, who understand the MR physics and the clinical questions to alter the acquisition parameters correctly.
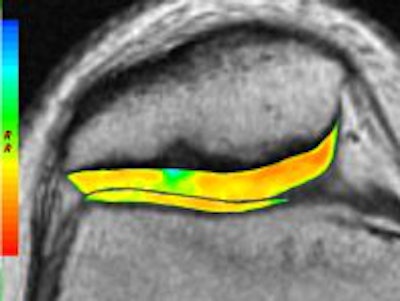
The philosophy is not to turn a noninvasive study into an invasive study. We use hardly any intra-articular contrast, but have changed the pulse sequence to the extent that we can visualize cartilage, which we see as one of the prime early determinants of arthritis, both osteoarthritis and inflammatory arthritis. This is something you want to visualize with exquisite detail.
We are doing T2 mapping and are doing special studies to try to evaluate cartilage changes at the microscopic level, at the occult level, before someone putting in an arthroscope would see it.
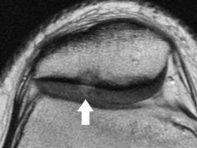 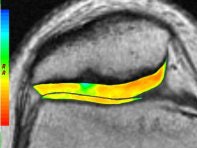 |
| Axial cartilage-sensitive fast-spin echo MR image (left) of the patellofemoral joint of the knee in an 18-year-old patient demonstrates focal signal hyperintensity of the articular cartilage (arrow) identified centrally in the lateral facet, with delamination from the deep components, starting at the radial zone adjacent to the tidemark. Note the associated deformity of the subchondral bone with sclerosis. Corresponding quantitative T2 relaxation time color map (right) coded to capture T2 values ranging from 10 to 90 msec, with green and blue reflecting longer T2 values, yellow intermediate, and orange the shorter values, demonstrates striking prolongation of T2 values over the basilar component at this site, which is an indication of breakdown in the collagen component of the extracellular matrix. Note that the thickness of the cartilage is unaffected. Images courtesy of the Hospital for Special Surgery. |
Similarly, with ultrasound, under the direction of the division chief Dr. Ronald Adler, we are investigating various ultrasound contrast agents that can help us detect vascularity patterns, both in normal, abnormal, and postsurgical situations, to try to determine patterns of healing. This is research that's still going on, with the potential to predict those patients postsurgically who are going to do well.
From a treatment aspect, ultrasound is fantastic. We are doing a lot of interventional musculoskeletal procedures in which you take somebody who has calcific tendinitis, or has a target zone of pain, and instead of going in blindly with a needle, like putting a needle into where it hurts and injecting a steroid, we do it under targeted ultrasound guidance. The radiologist knows exactly where it is going, we know exactly that if the patient gets better, that is the trigger point, and I think the patients are much better off for it.
Can you describe some of the technologies and techniques that you think are most exciting in each modality in musculoskeletal imaging?
In MR it's imaging around hardware, intra-articular imaging without intra-articular or intravenous contrast so it's noninvasive. With ultrasound it's being able to visualize -- without ionizing radiation -- patterns of inflammation, early detection of rheumatoid arthritis, and postsurgical healing patterns to see if healing is progressing appropriately.
In CR and DR, the main thing is trying to optimize image quality and patient throughput. It's basically converting from the world of analog to a world of digital. We have to find ways of making it as efficient as possible, both for the patient and for the department.
And the transition (to digital x-ray) is an issue, taking down a room, putting up a new room, and try to keep the workflow going while you've got down rooms.
With CR and DR, are you finding you're able to operate more efficiently, or is there still a bit of a learning curve?
I think we're always in a learning curve; however, increasing volume is an issue. Rooms have to come down (in order to convert to digital). Until we get all the rooms converted, we're in a situation where we don't have enough operational rooms. We are trying to do that in a staged program, and it seems to be working as best as possible.
DR definitely improves your patient turnaround. It's really nice, you're right there with the patient and you see the image. It's exactly like taking a photograph and determining immediately if it is a keeper or not.
Because we are an orthopedic hospital, however, we are still printing film. It will probably take some time for the orthopedic surgeons to change over and not need the film. Part of that is also that we are just deploying our PACS implementations and we don't have workstations or Web access yet, but we will, and we will get the surgeons more comfortable with filmless. But right now, that part of it is still difficult.
How are you seeing things split in terms of applications between CR and DR? What is DR good for, and what do you still want to use CR for?
You need to use CR for certain views. There are some views we can't do with the DR detectors as currently available, such as the axillary view, West Point view, or the Merchant view. You need to have CR capability -- you still need to put a cassette in an unusual location in order to get the desired image. I do think that some of the companies are making detectors with different kinds of mobile arms to accommodate that, but we are not at that stage yet.
What about nuclear medicine? Is that primarily useful for bone scanning?
It is primarily used for bone scanning, detection of early infection, trying to distinguish between infection and inflammatory conditions, like painful hardware, or arthroplasty. It's also useful when you see one lesion and you want to know if there are multiple lesions, if it's a metastatic disease process as opposed to a focused lesion.
In children, it's easier for a child to have a nuclear medicine study than an MR examination, especially in a younger child who may need to be sedated.
You don't see any reduction in the need for bone scanning in nuclear medicine?
At one point, I thought we did. When it came that we had to replace the machine we did consider closing the division, because MRI was taking over its venue. But there was a big outcry from the orthopedic surgeons who felt, no, they need bone scanning, and it's true. We got a new machine and the service is growing.
With PACS there is almost instantaneous access to images in that the referring physicians are getting them almost as fast as the radiologists do. Do you get any requests from the orthopedic physicians to get images more quickly, and how do you deal with that?
Well, the orthopedic surgeons would like to have their images before the patient has even entered the hospital. That would be ideal for them.
As I said, right now we are still printing films. Because they have access to images where they are acquired, we have noticed that some of the orthopedic surgeons will go over there to see the image before the film gets printed. I believe (PACS) is going to absolutely revolutionize how they do their practice, and certainly the younger guys who are computer savvy will find ways to use the images, downloading them for presentations and things a lot faster than the current system.
Instant access to images and access to images at multiple sites simultaneously will absolutely revolutionize things so that when they are looking at an image on plain film, we can pull it up and look at it at the same time, without somebody walking over to the other person's area, to discuss the findings.
So it will really improve the communication between radiology and orthopedics.
At HSS, communication between the surgeons and the radiologists is crucial and because we are a small hospital, there is excellent communication with patient images and clinical situation. PACS will just make it easier and less time-consuming.
Do you have conflicts with orthopedic surgeons who want to read the images themselves?
There are always conflicts. There are always turf wars. We are in a hospital, it's accredited by JCAHO (Joint Commission on Accreditation of Healthcare Organizations), and we are interpreting the images. Would they like to read their own films? Absolutely. But we value-add to the patient imaging exams, even on the plain films.
What happens when you have a surgeon who for the last 30 years all they do is knees? Can they detect an abnormality faster than you? They might think that they can. And they might do better than a junior radiologist, or somebody who may not be concentrating just on total knees or whatever the condition is.
But in general, radiology should -- and we try to -- value-add, so you are bringing something else to the table. You have to be very careful ... if you painted a picture and you're looking at it, you're not going to have the same critical eye as somebody else. If the surgeon is looking at a post-op image, they are looking at their own handiwork. There is always the sense of missing the little periosteal reaction that says that there is an infection or something going on because they are not going to focus in on it, they don't want to see it.
The bottom line is always finances. They like to be in control, most people do, and you have to provide something better that makes them want to seek your involvement. Imaging studies like MRI, nuclear medicine, and CT are a little more complicated to read. But we are dealing with very intelligent surgeons who are educable. And we are also constantly teaching them, and we are very good teachers. So it gets to the point where they feel they can do their own.
We must continually be improving what we do, so that they expect that we can give them more information than they can be able to see themselves.
What sort of advice do you have for radiologists out there in the imaging world who are dealing with conflicts with their referring physicians?
Don't be complacent. I think that if you are going to give them mediocre service and mediocre reports, and give them reports and say, "No abnormalities found," they will take it over, and justifiably so. You have to provide a service that says, yes, I went to medical school, I have more education in this area of specialty, and I'm going to identify for you things that you may not be aware of that will help you and your patients.
Anything else you see exciting in the world of musculoskeletal radiology that you plan to follow?
I think that as imaging keeps getting better and better and detail keeps getting more exquisite, and everything is faster and we have more diagnostic 3D reformations, I think what's going to happen is that we are going to be able to make diagnoses of conditions before patients are symptomatic from them, and hopefully be able to intervene more conservatively and with less downtime, as opposed to intervening with major surgical treatments because the situation is very dramatic and sometimes not really fixable.
With the arrival of technical advancements to permit molecular imaging, I think we'll be able to detect things at very, very early stages.
That's interesting, because when people talk about molecular imaging it's usually in the context of oncology. Where are applications in orthopedics?
MR will get there, especially as you get higher and higher tesla and can use (the scanners) safely. Ultrasound is already going in that direction with specific contrast agents (microbubbles) that allow you to visualize vascularity patterns that we've never visualized before.
We really don't do any PET scanning at HSS, because we primarily deal with sports injuries, arthritis, and arthroplasty and less with tumors. For me, that's where I see imaging going.
If you had to pick one technology and its potential to change musculoskeletal imaging, what would it be?
I would honestly have to say ultrasound and MRI, both of them. The thing you want to do is not lose the technology and potential technological advancements and applications to people who are going to use them just as a means of making money. I know that sounds pretty harsh, but the technologies are there -- you want to utilize them and enhance the imaging capacity to its potential.
By Brian Casey
AuntMinnie.com staff writer
February 17, 2006
Copyright © 2006 AuntMinnie.com